Hypocalcemia is a condition characterized by low calcium levels in the blood, leading to symptoms such as muscle cramps, tingling, and fatigue. It often results from vitamin D deficiency, kidney disorders, or parathyroid gland problems, requiring prompt diagnosis and treatment to avoid complications. Discover the causes, symptoms, and effective management strategies to protect Your health in the full article.
Table of Comparison
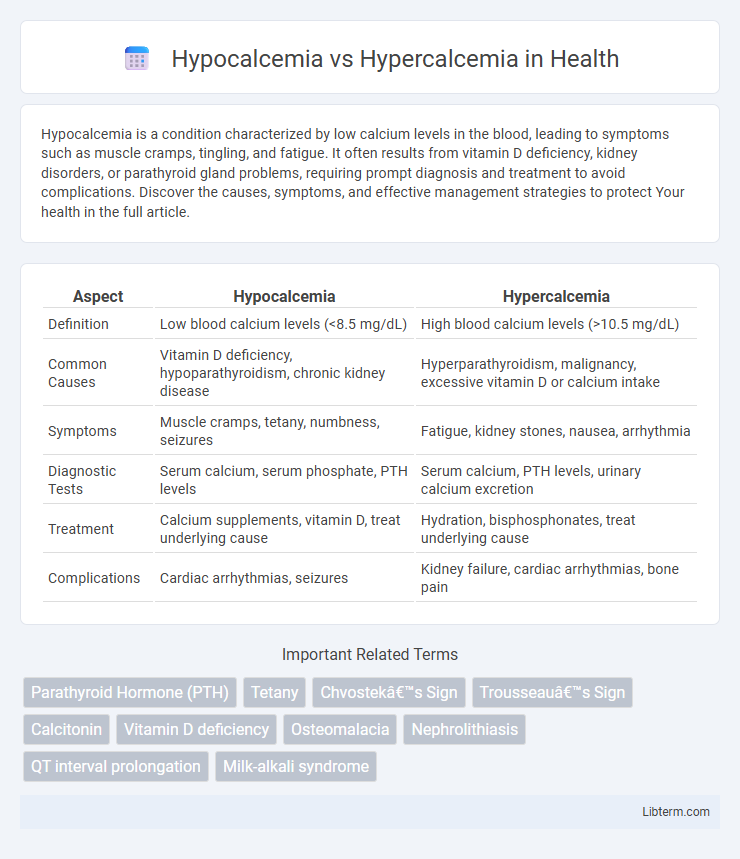
| Aspect | Hypocalcemia | Hypercalcemia |
|---|---|---|
| Definition | Low blood calcium levels (<8.5 mg/dL) | High blood calcium levels (>10.5 mg/dL) |
| Common Causes | Vitamin D deficiency, hypoparathyroidism, chronic kidney disease | Hyperparathyroidism, malignancy, excessive vitamin D or calcium intake |
| Symptoms | Muscle cramps, tetany, numbness, seizures | Fatigue, kidney stones, nausea, arrhythmia |
| Diagnostic Tests | Serum calcium, serum phosphate, PTH levels | Serum calcium, PTH levels, urinary calcium excretion |
| Treatment | Calcium supplements, vitamin D, treat underlying cause | Hydration, bisphosphonates, treat underlying cause |
| Complications | Cardiac arrhythmias, seizures | Kidney failure, cardiac arrhythmias, bone pain |
Introduction to Calcium Balance in the Body
Calcium balance in the body is tightly regulated by hormones such as parathyroid hormone, calcitonin, and vitamin D to maintain serum calcium levels within a narrow range of 8.5 to 10.2 mg/dL. Hypocalcemia occurs when serum calcium levels drop below this range, leading to neuromuscular irritability and cardiac dysfunction, while hypercalcemia results from elevated calcium levels, often causing muscle weakness, kidney stones, and altered mental status. Proper calcium homeostasis is essential for critical physiological functions including bone mineralization, blood clotting, and neuromuscular transmission.
Understanding Hypocalcemia: Definition and Causes
Hypocalcemia is defined as a lower-than-normal level of calcium in the blood, typically below 8.5 mg/dL, which is essential for nerve function, muscle contraction, and bone health. Common causes include hypoparathyroidism, vitamin D deficiency, chronic kidney disease, and certain medications like bisphosphonates or anticonvulsants. Accurate diagnosis involves serum calcium measurement, alongside assessing parathyroid hormone levels and vitamin D status to determine the underlying etiology.
Understanding Hypercalcemia: Definition and Causes
Hypercalcemia is characterized by an abnormally high concentration of calcium in the blood, typically exceeding 10.5 mg/dL. Common causes include hyperparathyroidism, malignancies such as lung or breast cancer, excessive vitamin D intake, and certain medications like thiazide diuretics. Understanding the underlying mechanisms of hypercalcemia is crucial for accurate diagnosis and effective treatment of this metabolic disorder.
Key Symptoms of Hypocalcemia
Hypocalcemia is characterized by symptoms such as muscle cramps, tetany, and paraesthesia, particularly around the lips and fingertips. Patients may also experience neurological manifestations like seizures, irritability, and cognitive disturbances due to low serum calcium levels. In contrast, hypercalcemia presents with symptoms including fatigue, nausea, polyuria, and kidney stones, highlighting the importance of distinguishing these calcium imbalances in clinical diagnosis.
Key Symptoms of Hypercalcemia
Hypercalcemia typically presents with symptoms such as nausea, vomiting, frequent urination, and excessive thirst, reflecting elevated calcium levels disrupting normal bodily functions. Patients may also experience muscle weakness, fatigue, confusion, and abdominal pain, which indicate the nervous system and gastrointestinal involvement. Severe hypercalcemia can lead to cardiac arrhythmias and kidney stones, emphasizing the need for prompt diagnosis and management.
Diagnostic Approaches: Hypocalcemia vs Hypercalcemia
Diagnostic approaches for hypocalcemia primarily involve serum calcium level measurement, ionized calcium testing, and evaluation of parathyroid hormone (PTH) levels to identify underlying causes such as hypoparathyroidism or vitamin D deficiency. Hypercalcemia diagnosis requires assessment of total and ionized calcium concentrations, PTH levels to distinguish primary hyperparathyroidism from malignancy-associated hypercalcemia, and imaging studies like sestamibi scans or bone surveys for tumor detection. Both conditions may necessitate additional tests including serum phosphate, magnesium, vitamin D metabolites, and renal function tests to fully understand the etiology and guide treatment strategies.
Common Risk Factors and Populations Affected
Hypocalcemia commonly affects individuals with chronic kidney disease, vitamin D deficiency, or hypoparathyroidism, while hypercalcemia is frequently seen in patients with hyperparathyroidism, malignancies, or excessive vitamin D intake. Risk factors for hypocalcemia include malnutrition, postoperative states (especially thyroid or parathyroid surgery), and certain medications like bisphosphonates and anticonvulsants. Hypercalcemia risk increases in older adults, those with osteoporosis on calcium supplements, and individuals with granulomatous diseases such as sarcoidosis.
Treatment Strategies for Hypocalcemia
Treatment strategies for hypocalcemia primarily involve calcium supplementation, either orally or intravenously, depending on severity. Vitamin D analogs, such as calcitriol, are often prescribed to enhance calcium absorption and maintain stable serum calcium levels. Monitoring magnesium levels is crucial, as hypomagnesemia can impair calcium regulation and complicate treatment efficacy.
Treatment Strategies for Hypercalcemia
Treatment strategies for hypercalcemia primarily focus on lowering elevated serum calcium levels through hydration with intravenous saline to increase renal calcium excretion and the use of bisphosphonates like pamidronate or zoledronic acid to inhibit bone resorption. In severe cases, calcitonin may provide rapid but temporary reduction of calcium levels, while corticosteroids are effective in hypercalcemia caused by granulomatous diseases or malignancies. Dialysis can be considered for patients with renal failure or refractory hypercalcemia when conventional treatments are insufficient.
Prevention and Long-term Management
Preventing hypocalcemia involves maintaining adequate dietary calcium and vitamin D intake, monitoring at-risk populations such as post-surgical patients or those with hypoparathyroidism, and managing underlying conditions like chronic kidney disease. Long-term management of hypocalcemia requires regular serum calcium monitoring, supplementation with calcium and active vitamin D analogs, and addressing contributing factors like magnesium deficiency. For hypercalcemia, prevention centers on managing hyperparathyroidism, minimizing excessive calcium or vitamin D intake, and careful use of medications that affect calcium metabolism; chronic management includes treating the underlying cause, hydration, bisphosphonates, and monitoring for complications such as kidney stones or cardiac arrhythmias.
Hypocalcemia Infographic
 libterm.com
libterm.com