Necrosis refers to the premature death of cells in living tissue caused by factors such as infection, toxins, or trauma, leading to inflammation and tissue damage. This process disrupts normal cellular function and can result in severe health complications if untreated. Explore the rest of the article to understand the causes, symptoms, and treatment options for necrosis and how it might affect your health.
Table of Comparison
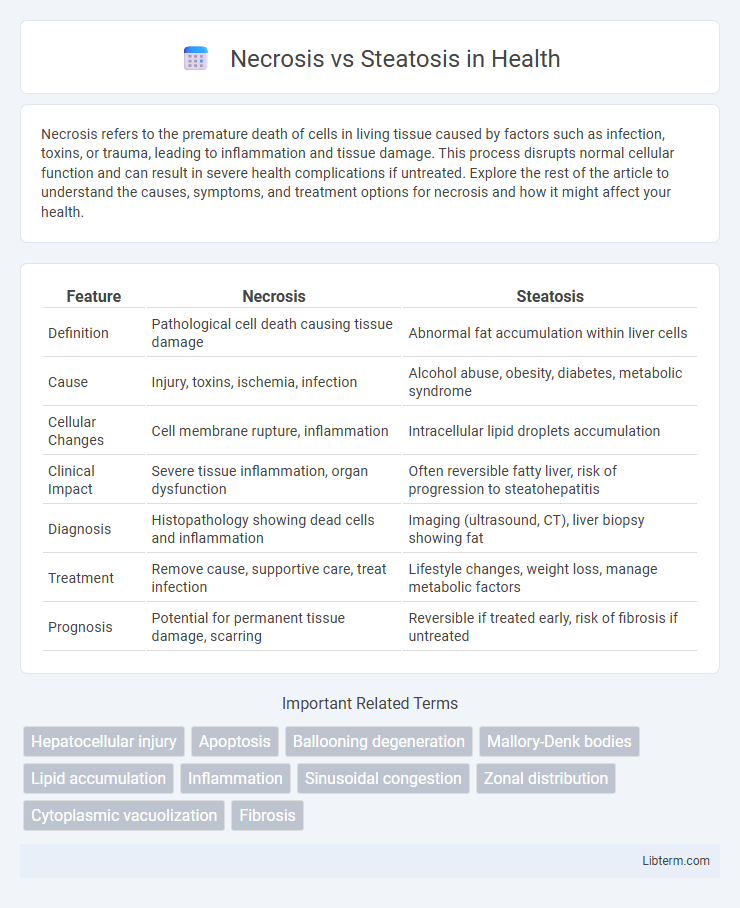
| Feature | Necrosis | Steatosis |
|---|---|---|
| Definition | Pathological cell death causing tissue damage | Abnormal fat accumulation within liver cells |
| Cause | Injury, toxins, ischemia, infection | Alcohol abuse, obesity, diabetes, metabolic syndrome |
| Cellular Changes | Cell membrane rupture, inflammation | Intracellular lipid droplets accumulation |
| Clinical Impact | Severe tissue inflammation, organ dysfunction | Often reversible fatty liver, risk of progression to steatohepatitis |
| Diagnosis | Histopathology showing dead cells and inflammation | Imaging (ultrasound, CT), liver biopsy showing fat |
| Treatment | Remove cause, supportive care, treat infection | Lifestyle changes, weight loss, manage metabolic factors |
| Prognosis | Potential for permanent tissue damage, scarring | Reversible if treated early, risk of fibrosis if untreated |
Introduction to Necrosis and Steatosis
Necrosis is the pathological process involving the premature death of cells in living tissue due to injury, infection, or toxins, characterized by cell swelling, membrane rupture, and inflammation. Steatosis, commonly referred to as fatty liver, is the abnormal accumulation of lipids within hepatocytes, often resulting from metabolic imbalances, alcohol abuse, or obesity. Both conditions represent distinct cellular responses to stress, with necrosis leading to irreversible tissue damage and steatosis primarily indicating reversible lipid accumulation.
Defining Necrosis: Causes and Characteristics
Necrosis is characterized by the uncontrolled death of cells due to factors such as ischemia, toxins, or infections, leading to inflammation and tissue damage. This pathological process results in cell membrane rupture, mitochondrial dysfunction, and the release of intracellular contents, triggering an immune response. In contrast, steatosis involves the accumulation of fat within liver cells, often caused by metabolic imbalances like obesity, diabetes, or alcohol abuse, without immediate cell death or inflammation.
Understanding Steatosis: Types and Mechanisms
Steatosis, characterized by abnormal accumulation of triglycerides within hepatocytes, is classified primarily into macrovesicular and microvesicular types, each differing in lipid droplet size and distribution. Macrovesicular steatosis involves large lipid droplets displacing the nucleus, often linked to alcohol abuse and metabolic syndrome, while microvesicular steatosis features small lipid droplets without nuclear displacement, commonly associated with mitochondrial dysfunction and toxic injury. Understanding these mechanisms highlights disruptions in lipid metabolism, including impaired beta-oxidation and increased lipid synthesis, distinguishing steatosis from necrosis, which involves irreversible cell death and tissue destruction.
Key Differences Between Necrosis and Steatosis
Necrosis is characterized by uncontrolled cell death resulting from injury, causing inflammation and tissue damage, whereas steatosis involves abnormal lipid accumulation within cells, primarily hepatocytes, without immediate cell death. Necrosis leads to cell membrane rupture and release of intracellular contents, triggering inflammatory responses, while steatosis presents as reversible fat deposition often related to metabolic dysfunction or alcohol use. The key distinction lies in necrosis representing a pathological endpoint involving cell destruction, whereas steatosis reflects a cellular metabolic imbalance preceding potential progression to liver injury.
Cellular Changes in Necrosis vs Steatosis
Necrosis involves irreversible cellular damage characterized by plasma membrane rupture, organelle swelling, and loss of nuclear integrity, leading to cell death and inflammation. In contrast, steatosis is marked by the accumulation of lipid droplets within the cytoplasm, causing cellular enlargement without immediate membrane disruption or cell death. Cellular changes in necrosis result in leakage of intracellular contents, while steatosis primarily represents reversible lipid metabolic dysfunction.
Common Causes and Risk Factors
Necrosis commonly results from ischemia, infections, toxins, and trauma leading to unregulated cell death, whereas steatosis primarily arises from alcohol abuse, obesity, diabetes, and metabolic syndrome causing abnormal fat accumulation in liver cells. Risk factors for necrosis include prolonged hypoxia, viral hepatitis, and exposure to hepatotoxic drugs, while steatosis risk factors emphasize insulin resistance, high-fat diets, and sedentary lifestyles. Understanding these distinct causes helps in diagnosing liver conditions and guiding appropriate therapeutic interventions.
Clinical Manifestations and Diagnosis
Necrosis presents clinically with severe pain, signs of inflammation, and possible systemic symptoms such as fever and leukocytosis, often reflecting irreversible cell injury and tissue death. In contrast, steatosis is typically asymptomatic and detected incidentally through imaging or elevated liver enzymes, indicating reversible fat accumulation within hepatocytes. Diagnosis of necrosis relies on histopathological examination showing cell membrane disruption and inflammation, while steatosis is confirmed by imaging techniques like ultrasound or MRI and liver biopsy revealing intracellular lipid vacuoles.
Pathological Consequences and Prognosis
Necrosis involves irreversible cell death causing tissue destruction and provoking intense inflammatory responses, often leading to impaired organ function and poor prognosis if extensive. Steatosis, characterized by abnormal lipid accumulation within hepatocytes, generally represents a reversible condition but can progress to steatohepatitis, fibrosis, and cirrhosis, worsening long-term outcomes. The pathological consequences of necrosis are typically more acute and severe, while steatosis poses a chronic risk with potential for gradual liver damage and metabolic complications.
Treatment Approaches for Necrosis and Steatosis
Treatment for necrosis involves immediate interventions such as surgical debridement, antibiotics to prevent infection, and supportive care to restore blood flow and oxygenation to affected tissues. Steatosis management primarily centers on lifestyle modifications including dietary changes, weight loss, and controlling underlying conditions like diabetes or hyperlipidemia to reduce fat accumulation in the liver. Pharmacological therapies targeting metabolic pathways and antioxidants are also explored to improve liver function in steatosis patients.
Prevention Strategies and Future Research
Preventing necrosis involves minimizing exposure to toxins, controlling ischemia, and managing underlying conditions such as infections or metabolic disorders. Steatosis prevention prioritizes lifestyle modifications including balanced diets and regular exercise to reduce lipid accumulation in liver cells. Future research targets molecular pathways mediating cell death and fat metabolism, aiming to develop targeted therapies that can halt or reverse these pathological processes.
Necrosis Infographic
 libterm.com
libterm.com