Transcatheter aortic valve implantation (TAVI) is a minimally invasive procedure designed to replace a narrowed aortic valve that fails to open properly, improving blood flow and reducing symptoms of aortic stenosis. This technique is particularly beneficial for patients at high risk for traditional open-heart surgery, offering quicker recovery and fewer complications. Discover how TAVI can transform your treatment options and enhance your quality of life by reading the full article.
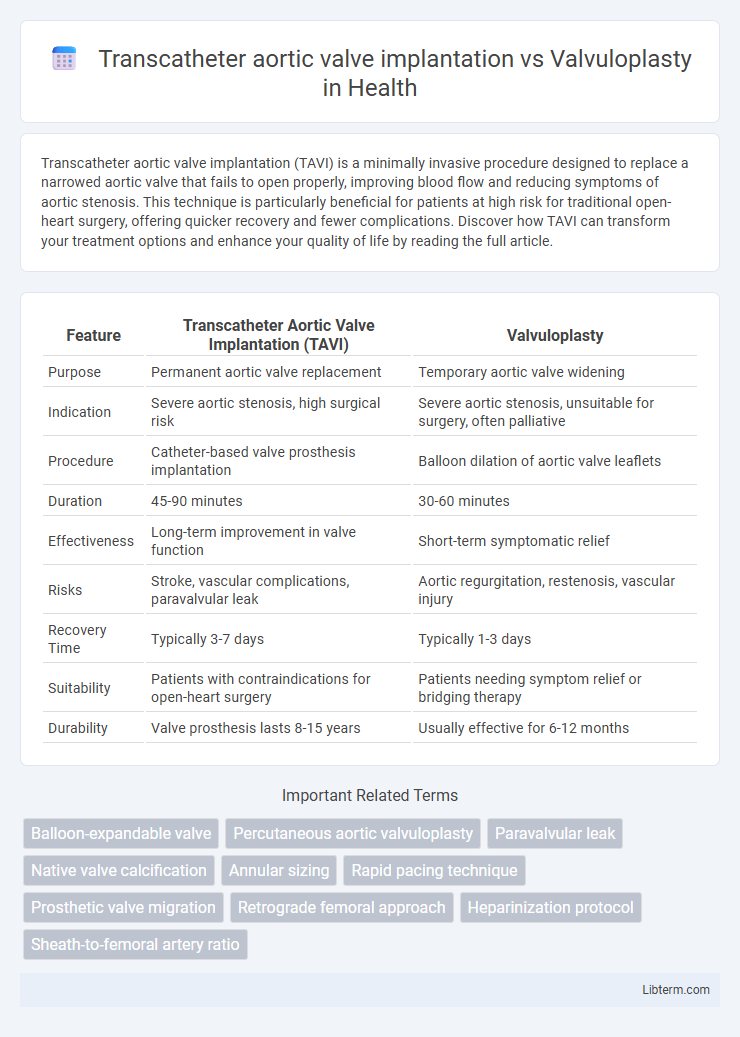
Table of Comparison
| Feature | Transcatheter Aortic Valve Implantation (TAVI) | Valvuloplasty |
|---|---|---|
| Purpose | Permanent aortic valve replacement | Temporary aortic valve widening |
| Indication | Severe aortic stenosis, high surgical risk | Severe aortic stenosis, unsuitable for surgery, often palliative |
| Procedure | Catheter-based valve prosthesis implantation | Balloon dilation of aortic valve leaflets |
| Duration | 45-90 minutes | 30-60 minutes |
| Effectiveness | Long-term improvement in valve function | Short-term symptomatic relief |
| Risks | Stroke, vascular complications, paravalvular leak | Aortic regurgitation, restenosis, vascular injury |
| Recovery Time | Typically 3-7 days | Typically 1-3 days |
| Suitability | Patients with contraindications for open-heart surgery | Patients needing symptom relief or bridging therapy |
| Durability | Valve prosthesis lasts 8-15 years | Usually effective for 6-12 months |
Introduction to Aortic Valve Interventions
Transcatheter aortic valve implantation (TAVI) and valvuloplasty are minimally invasive procedures designed to treat aortic valve stenosis, a condition characterized by the narrowing of the aortic valve opening. TAVI involves the replacement of the diseased valve with a prosthetic valve via catheter-based techniques, offering a definitive solution for severe aortic stenosis, especially in patients at high surgical risk. Valvuloplasty uses balloon dilation to temporarily relieve valve obstruction but generally serves as a palliative or bridge therapy due to limited long-term efficacy compared to TAVI.
Understanding Transcatheter Aortic Valve Implantation (TAVI)
Transcatheter Aortic Valve Implantation (TAVI) offers a minimally invasive alternative to surgical valve replacement for patients with severe aortic stenosis, delivering a bioprosthetic valve through catheter-based techniques. Unlike balloon valvuloplasty, which temporarily dilates a narrowed aortic valve, TAVI provides a durable and long-term solution by permanently replacing the diseased valve. Outcomes data show TAVI improves survival and quality of life in high-risk and inoperable patients, making it a preferred choice in contemporary cardiology practice.
What Is Aortic Valvuloplasty?
Aortic valvuloplasty is a minimally invasive procedure that involves balloon dilation to widen a narrowed aortic valve, primarily used to temporarily relieve severe aortic stenosis. Unlike transcatheter aortic valve implantation (TAVI), which replaces the valve, valvuloplasty aims to improve valve function without the insertion of a new valve, often serving as a bridge to more definitive treatment. This technique is frequently applied in patients who are high-risk surgical candidates or as an interim measure before TAVI or surgical valve replacement.
Indications for TAVI vs Valvuloplasty
Transcatheter aortic valve implantation (TAVI) is primarily indicated for patients with severe symptomatic aortic stenosis who are at high or prohibitive surgical risk, including elderly patients or those with multiple comorbidities. Valvuloplasty is generally reserved for patients with symptomatic aortic stenosis who are not candidates for surgery or TAVI, often serving as a palliative or bridging procedure to improve symptoms temporarily. TAVI provides a more durable solution with improved survival rates compared to valvuloplasty, which tends to have limited long-term efficacy due to restenosis.
Patient Selection Criteria
Patient selection for transcatheter aortic valve implantation (TAVI) centers on patients with severe symptomatic aortic stenosis who are considered high or intermediate surgical risk due to advanced age, comorbidities, or frailty. Balloon aortic valvuloplasty (BAV) serves primarily as a palliative or bridge therapy for patients with prohibitive surgical risk or hemodynamic instability but typically offers only temporary relief. Key criteria for TAVI include anatomical suitability assessed by imaging modalities like CT angiography, while BAV is often reserved when TAVI or surgical valve replacement is contraindicated or delayed.
Procedural Techniques and Differences
Transcatheter aortic valve implantation (TAVI) involves the deployment of a bioprosthetic valve via a catheter, usually through the femoral artery, allowing precise placement and immediate valve function restoration. Valvuloplasty utilizes balloon dilation to temporarily widen the stenotic aortic valve, offering symptomatic relief but often followed by restenosis due to the lack of valve replacement. TAVI provides a more durable solution with reduced long-term complications, whereas valvuloplasty is primarily a palliative or bridge therapy in high-risk patients.
Clinical Outcomes and Long-Term Results
Transcatheter aortic valve implantation (TAVI) demonstrates superior clinical outcomes compared to balloon valvuloplasty, including lower rates of restenosis and improved valve function over time. Long-term results from randomized controlled trials indicate that TAVI significantly reduces mortality and rehospitalization rates in patients with severe aortic stenosis. In contrast, valvuloplasty is associated with transient symptomatic relief but higher incidence of valve restenosis and the need for repeat interventions.
Risks and Complications Comparison
Transcatheter aortic valve implantation (TAVI) typically carries a lower risk of restenosis and valve regurgitation compared to balloon valvuloplasty, which often requires repeat procedures due to valve recoil. TAVI is associated with complications such as vascular injury, stroke, and conduction disturbances leading to permanent pacemaker implantation, whereas valvuloplasty poses a higher risk of acute aortic regurgitation and procedural embolization. Meta-analyses reveal that TAVI offers improved long-term survival and fewer repeat interventions despite a slightly elevated risk of vascular complications relative to valvuloplasty.
Recovery, Follow-Up, and Quality of Life
Transcatheter aortic valve implantation (TAVI) offers faster recovery times with most patients resuming normal activities within weeks, unlike balloon valvuloplasty which often requires repeat procedures due to restenosis. Follow-up for TAVI includes regular echocardiograms to monitor valve function and prevent complications such as paravalvular leak, whereas valvuloplasty follow-up focuses on tracking aortic valve gradient recurrence. Quality of life after TAVI significantly improves with reduced symptoms of aortic stenosis, while valvuloplasty typically provides only temporary symptomatic relief, leading to variable long-term outcomes.
Future Perspectives in Aortic Valve Therapies
Transcatheter aortic valve implantation (TAVI) continues to advance with innovations such as improved valve designs and delivery systems, promising enhanced durability and expanded eligibility for lower-risk patients. Valvuloplasty, while primarily a palliative intervention, is being re-evaluated as a bridge to TAVI or surgical replacement in complex cases with emerging balloon technologies improving procedural safety. Future perspectives in aortic valve therapies emphasize integration of personalized treatment algorithms, combining TAVI advancements and refined valvuloplasty techniques to optimize outcomes for diverse patient populations.
Transcatheter aortic valve implantation Infographic
 libterm.com
libterm.com