Dehydration occurs when your body loses more fluids than it takes in, disrupting essential physiological functions. Symptoms such as dizziness, fatigue, and dry mouth signal the urgent need to replenish lost water to maintain optimal health. Explore the rest of this article to learn effective ways to prevent dehydration and recognize its warning signs.
Table of Comparison
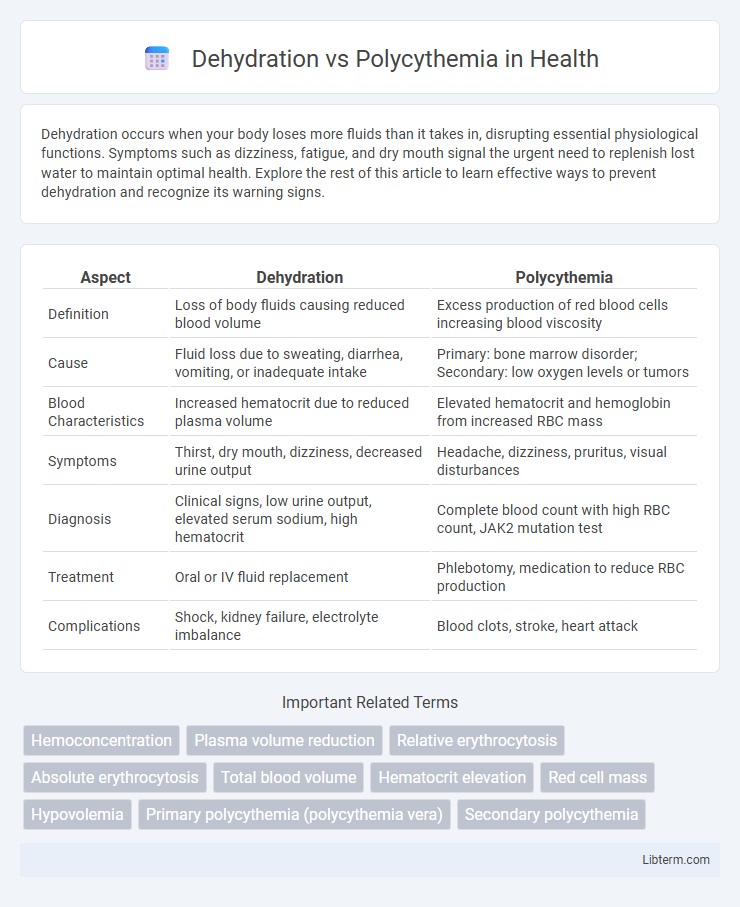
| Aspect | Dehydration | Polycythemia |
|---|---|---|
| Definition | Loss of body fluids causing reduced blood volume | Excess production of red blood cells increasing blood viscosity |
| Cause | Fluid loss due to sweating, diarrhea, vomiting, or inadequate intake | Primary: bone marrow disorder; Secondary: low oxygen levels or tumors |
| Blood Characteristics | Increased hematocrit due to reduced plasma volume | Elevated hematocrit and hemoglobin from increased RBC mass |
| Symptoms | Thirst, dry mouth, dizziness, decreased urine output | Headache, dizziness, pruritus, visual disturbances |
| Diagnosis | Clinical signs, low urine output, elevated serum sodium, high hematocrit | Complete blood count with high RBC count, JAK2 mutation test |
| Treatment | Oral or IV fluid replacement | Phlebotomy, medication to reduce RBC production |
| Complications | Shock, kidney failure, electrolyte imbalance | Blood clots, stroke, heart attack |
Understanding Dehydration: Definition and Causes
Dehydration occurs when the body loses more fluids than it takes in, leading to an imbalance in electrolytes and reduced blood volume. Common causes include excessive sweating, vomiting, diarrhea, and inadequate fluid intake, which disrupt normal cellular functions. Unlike polycythemia, which involves an increased red blood cell concentration, dehydration primarily results in hemoconcentration due to fluid loss rather than abnormal blood cell production.
What is Polycythemia? Types and Overview
Polycythemia is a condition characterized by an increased concentration of red blood cells in the bloodstream, leading to thickened blood and impaired circulation. It is primarily classified into two types: primary polycythemia, also known as polycythemia vera, a myeloproliferative disorder caused by a mutation in the JAK2 gene resulting in uncontrolled red blood cell production; and secondary polycythemia, which arises due to chronic hypoxia or elevated erythropoietin levels from conditions like chronic lung disease or living at high altitudes. Understanding the distinction between these types is critical for accurate diagnosis and treatment, as primary polycythemia involves bone marrow pathology while secondary is a physiological response to oxygen deprivation.
Key Differences Between Dehydration and Polycythemia
Dehydration primarily involves a significant loss of body water resulting in reduced plasma volume and concentrated blood, whereas polycythemia is characterized by an abnormal increase in red blood cell mass, elevating blood viscosity. Key differences include that dehydration causes hemoconcentration due to fluid deficit, leading to high hematocrit and hemoglobin levels without an actual increase in red blood cell production, while polycythemia involves true overproduction or reduced destruction of red blood cells. Clinical diagnosis uses parameters such as plasma volume, red blood cell count, erythropoietin levels, and hydration status to differentiate between these conditions.
Shared Symptoms: How to Tell Them Apart
Dehydration and polycythemia both cause symptoms like fatigue, dizziness, and headache due to reduced blood volume or increased red blood cell count. Dehydration typically presents with dry mouth, decreased urination, and low blood pressure, while polycythemia often shows elevated hematocrit levels, redness of the skin, and high blood viscosity. Laboratory tests measuring serum osmolality, hemoglobin concentration, and red blood cell mass help differentiate these conditions accurately.
Diagnosis: Laboratory Tests and Clinical Evaluation
Diagnosis of dehydration primarily involves laboratory tests such as serum electrolytes, blood urea nitrogen (BUN), and hematocrit levels, which typically show elevated values due to hemoconcentration. In contrast, polycythemia diagnosis focuses on complete blood count (CBC) revealing increased red blood cell mass, elevated hemoglobin, and hematocrit, alongside erythropoietin levels to differentiate between primary and secondary causes. Clinical evaluation for dehydration assesses signs of fluid loss like dry mucous membranes and decreased skin turgor, whereas polycythemia evaluation includes symptoms of hyperviscosity such as headache, dizziness, and splenomegaly.
Risk Factors for Dehydration and Polycythemia
Risk factors for dehydration include prolonged exposure to high temperatures, excessive physical activity, inadequate fluid intake, and underlying medical conditions such as diabetes or gastrointestinal illnesses causing vomiting and diarrhea. Polycythemia risk factors involve chronic hypoxia from smoking or lung disease, genetic mutations like JAK2 gene mutation, and secondary causes such as tumors producing erythropoietin. Both conditions elevate blood viscosity, but dehydration primarily results from fluid loss, while polycythemia stems from increased red blood cell production.
Complications Associated with Each Condition
Dehydration commonly leads to complications such as hypovolemic shock, kidney failure, and electrolyte imbalances that can cause cardiac arrhythmias. Polycythemia increases the risk of thrombotic events, including stroke, myocardial infarction, and deep vein thrombosis, due to elevated blood viscosity and red blood cell mass. Both conditions require careful management to prevent severe vascular and organ damage.
Treatment Approaches: Hydration vs Medical Intervention
Dehydration treatment primarily involves rapid rehydration using oral or intravenous fluids to restore plasma volume and electrolyte balance, while polycythemia requires specific medical interventions such as phlebotomy, which reduces red blood cell mass, and medications like hydroxyurea to suppress bone marrow production. In cases of polycythemia vera, targeted therapies including JAK2 inhibitors are employed to manage abnormal cell proliferation. Effective management depends on accurately distinguishing between these conditions, as hydration alone can exacerbate complications in polycythemia patients.
Prevention Strategies for Dehydration and Polycythemia
Preventing dehydration involves maintaining adequate fluid intake, especially in hot climates and during physical activity, to preserve plasma volume and avoid hemoconcentration. Polycythemia prevention focuses on managing underlying causes, such as controlling smoking cessation and treating chronic hypoxia or sleep apnea, to reduce excessive red blood cell production. Regular monitoring of hematocrit and hemoglobin levels helps in early detection and effective management of both conditions.
When to Seek Medical Attention
Seek medical attention for dehydration if symptoms include extreme thirst, dizziness, rapid heartbeat, or confusion, as these indicate severe fluid loss requiring immediate treatment. In polycythemia, consult a healthcare provider when experiencing persistent headaches, blurred vision, or unexplained bleeding, which may signal elevated red blood cell levels and increased risk of blood clots. Early diagnosis and management of both conditions are crucial to prevent serious complications such as organ damage or stroke.
Dehydration Infographic
 libterm.com
libterm.com