Tachycardia is a condition characterized by an abnormally fast heart rate, typically over 100 beats per minute, which can lead to symptoms like dizziness, shortness of breath, and chest pain. Understanding the causes, such as stress, heart conditions, or medication side effects, is crucial for effective management and treatment. Explore the rest of the article to learn how you can recognize tachycardia symptoms and the best approaches to care for your heart health.
Table of Comparison
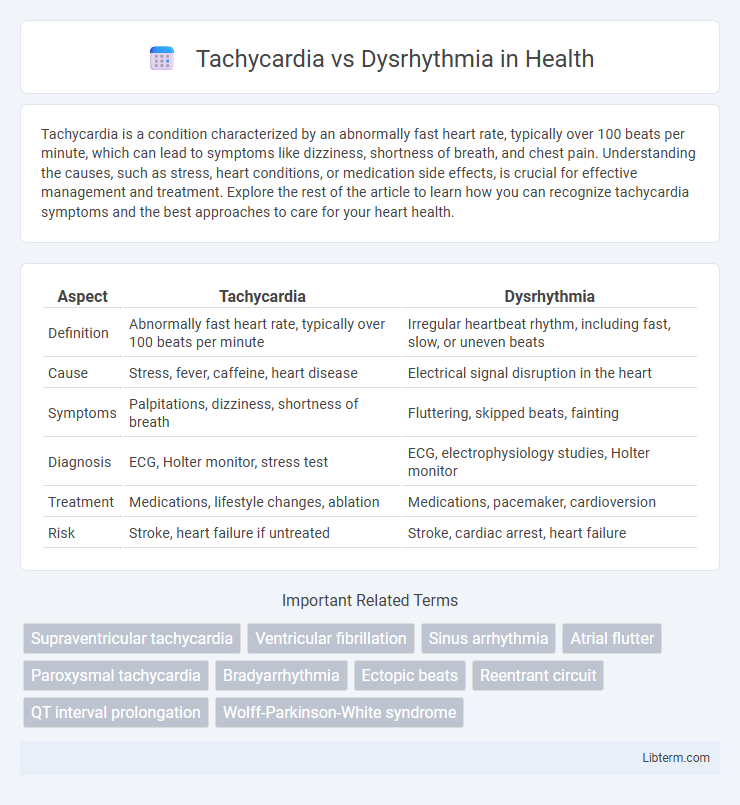
| Aspect | Tachycardia | Dysrhythmia |
|---|---|---|
| Definition | Abnormally fast heart rate, typically over 100 beats per minute | Irregular heartbeat rhythm, including fast, slow, or uneven beats |
| Cause | Stress, fever, caffeine, heart disease | Electrical signal disruption in the heart |
| Symptoms | Palpitations, dizziness, shortness of breath | Fluttering, skipped beats, fainting |
| Diagnosis | ECG, Holter monitor, stress test | ECG, electrophysiology studies, Holter monitor |
| Treatment | Medications, lifestyle changes, ablation | Medications, pacemaker, cardioversion |
| Risk | Stroke, heart failure if untreated | Stroke, cardiac arrest, heart failure |
Understanding Tachycardia: Definition and Types
Tachycardia refers to a condition characterized by an abnormally fast heart rate, typically exceeding 100 beats per minute in adults, with several types including atrial, ventricular, and sinus tachycardia distinguished by their origin within the heart's electrical conduction system. Understanding tachycardia involves recognizing its causes such as stress, heart disease, or electrolyte imbalances, and differentiating it from general dysrhythmia, which encompasses any irregular heart rhythm including bradycardia and arrhythmias. Proper identification of tachycardia types is crucial for effective treatment and management, as some forms like ventricular tachycardia may require immediate medical intervention.
What Is Dysrhythmia? A Comprehensive Overview
Dysrhythmia refers to any abnormality in the heart's rhythm, encompassing a range of irregular heartbeats including tachycardia, bradycardia, and arrhythmias caused by improper electrical conduction. This condition results from disruptions in the sinoatrial node, atrioventricular node, or His-Purkinje system, leading to irregular timing or sequence of heartbeats. Understanding dysrhythmia is crucial for diagnosing cardiac dysfunctions and preventing complications such as stroke, heart failure, and sudden cardiac arrest.
Causes of Tachycardia vs Dysrhythmias
Tachycardia arises from causes such as physiological stress, fever, anemia, hyperthyroidism, and cardiac conditions including ischemia or heart failure. Dysrhythmias result from structural heart disease, electrolyte imbalances, drug toxicity, and hereditary channelopathies. Both conditions share overlapping triggers but differ in underlying pathophysiological mechanisms, with tachycardia primarily involving increased heart rate and dysrhythmias encompassing abnormal heart rhythms.
Signs and Symptoms: How Tachycardia Differs from Dysrhythmia
Tachycardia is characterized by an abnormally fast heart rate exceeding 100 beats per minute, often causing palpitations, dizziness, and shortness of breath, whereas dysrhythmia refers to any irregular heart rhythm that may be too fast, too slow, or erratic, presenting symptoms such as skipped beats, fatigue, and chest discomfort. Tachycardia's rapid heartbeat is a specific subgroup of dysrhythmias, which encompass a broader range of arrhythmias including atrial fibrillation and ventricular flutter. Identifying these distinct symptoms is crucial for accurate diagnosis and targeted treatment of each cardiac condition.
Diagnostic Approaches: Identifying Tachycardia and Dysrhythmia
Electrocardiogram (ECG) remains the primary diagnostic tool to differentiate tachycardia, characterized by a heart rate exceeding 100 beats per minute, from dysrhythmia, which involves irregular or abnormal heart rhythms. Holter monitoring provides extended cardiac rhythm data, improving detection accuracy of intermittent dysrhythmias and episodes of tachycardia. Advanced diagnostics such as electrophysiological studies offer detailed mapping of cardiac electrical activity to identify the precise origin and mechanism of arrhythmic events.
Underlying Risk Factors and Triggers
Tachycardia, characterized by an abnormally fast heart rate above 100 beats per minute, often arises from underlying risk factors such as cardiovascular disease, electrolyte imbalances, and chronic stress. Dysrhythmia, a broader term encompassing any irregular heart rhythm, can be triggered by conditions like ischemic heart disease, structural heart abnormalities, and medication side effects. Both conditions share common triggers including caffeine, alcohol, smoking, and acute infections, which exacerbate the heart's electrical instability.
Treatment Options for Tachycardia vs Dysrhythmia
Treatment options for tachycardia typically include medications such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs, as well as procedures like catheter ablation to restore normal heart rhythm. Dysrhythmia management encompasses similar strategies, with an emphasis on identifying the specific type of arrhythmia to tailor therapy; options include lifestyle modifications, implantable devices like pacemakers or defibrillators, and pharmacological interventions. Both conditions may require emergency interventions such as electrical cardioversion in acute cases to prevent complications like stroke or heart failure.
Complications and Prognosis: Long-Term Outlook
Tachycardia and dysrhythmia both increase the risk of serious cardiovascular complications such as stroke, heart failure, and sudden cardiac arrest. The long-term prognosis depends on the underlying cause, frequency, and duration of arrhythmic episodes, with untreated tachycardia leading to tachycardia-induced cardiomyopathy. Effective management and timely intervention improve survival rates and reduce morbidity by preventing structural heart damage and maintaining normal heart rhythm.
Prevention Strategies for Cardiac Arrhythmias
Effective prevention strategies for cardiac arrhythmias such as tachycardia and dysrhythmia emphasize lifestyle modifications including regular physical activity, a heart-healthy diet low in sodium and saturated fats, and stress management techniques. Controlling risk factors such as hypertension, diabetes, and sleep apnea through medication adherence and routine monitoring reduces the incidence of abnormal heart rhythms. Avoiding stimulants like caffeine, tobacco, and excessive alcohol also plays a critical role in minimizing triggers for tachycardia and other dysrhythmias.
When to Seek Medical Attention: Warning Signs
Persistent heart rates above 100 beats per minute or irregular heartbeats accompanied by chest pain, dizziness, or shortness of breath require immediate medical evaluation to rule out tachycardia or dysrhythmia complications. Sudden onset of palpitations, fainting episodes, or extreme fatigue also signals urgent need for professional assessment. Early intervention in abnormal heart rhythms reduces risks of stroke, heart failure, or sudden cardiac arrest.
Tachycardia Infographic
 libterm.com
libterm.com