Atrial fibrillation is a common heart rhythm disorder characterized by rapid and irregular beating of the atria, increasing the risk of stroke and heart failure. Effective management includes medications, lifestyle changes, and sometimes procedural interventions to restore normal rhythm. Explore the rest of the article to understand how you can recognize symptoms and take proactive steps in managing atrial fibrillation.
Table of Comparison
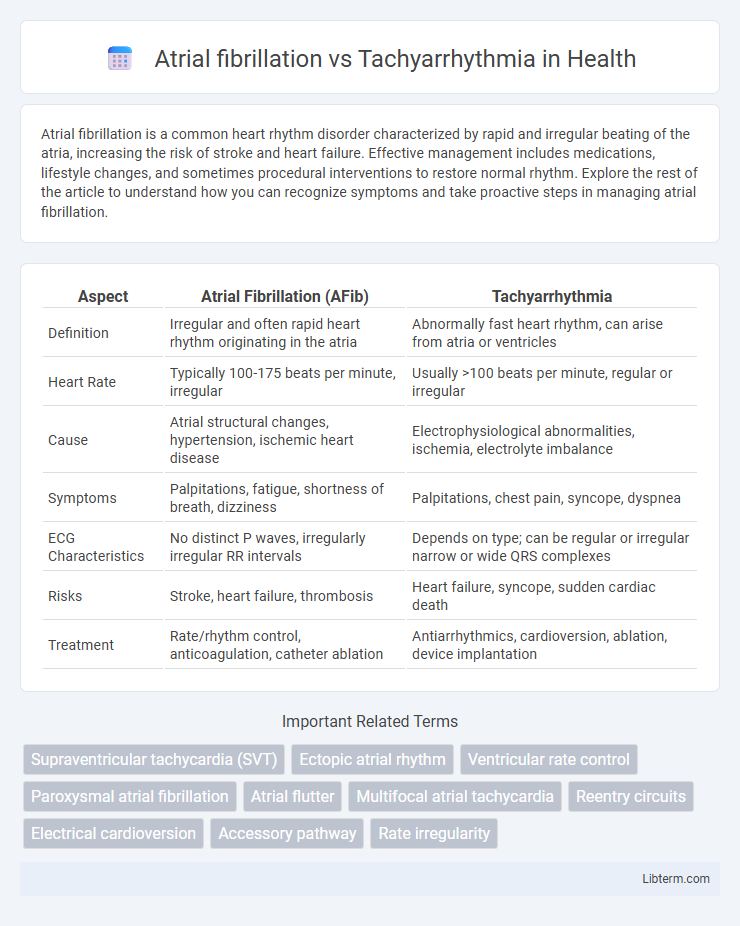
| Aspect | Atrial Fibrillation (AFib) | Tachyarrhythmia |
|---|---|---|
| Definition | Irregular and often rapid heart rhythm originating in the atria | Abnormally fast heart rhythm, can arise from atria or ventricles |
| Heart Rate | Typically 100-175 beats per minute, irregular | Usually >100 beats per minute, regular or irregular |
| Cause | Atrial structural changes, hypertension, ischemic heart disease | Electrophysiological abnormalities, ischemia, electrolyte imbalance |
| Symptoms | Palpitations, fatigue, shortness of breath, dizziness | Palpitations, chest pain, syncope, dyspnea |
| ECG Characteristics | No distinct P waves, irregularly irregular RR intervals | Depends on type; can be regular or irregular narrow or wide QRS complexes |
| Risks | Stroke, heart failure, thrombosis | Heart failure, syncope, sudden cardiac death |
| Treatment | Rate/rhythm control, anticoagulation, catheter ablation | Antiarrhythmics, cardioversion, ablation, device implantation |
Understanding Atrial Fibrillation and Tachyarrhythmia
Atrial fibrillation is a specific type of tachyarrhythmia characterized by rapid, irregular electrical impulses in the atria, leading to an irregular heartbeat and increased risk of stroke. Tachyarrhythmia broadly refers to any abnormally fast heart rhythm, including conditions like atrial fibrillation, ventricular tachycardia, and supraventricular tachycardia, each with distinct pathophysiology and clinical implications. Understanding the electrophysiological mechanisms and diagnostic criteria of atrial fibrillation versus other tachyarrhythmias is crucial for targeted management and effective treatment strategies.
Key Differences in Cardiac Rhythm
Atrial fibrillation is characterized by rapid, irregular atrial contractions causing disorganized electrical signals, whereas tachyarrhythmia refers to any fast heart rhythm exceeding 100 beats per minute, including both regular and irregular patterns. The key distinction lies in atrial fibrillation's hallmark irregularly irregular rhythm and absence of distinct P waves on ECG, while tachyarrhythmia encompasses a broader category such as ventricular tachycardia and supraventricular tachycardia, often with more regular rhythms. Understanding these differences is critical for diagnosis and targeted treatment strategies in arrhythmia management.
Common Causes and Risk Factors
Atrial fibrillation, characterized by irregular and often rapid heartbeats, commonly results from hypertension, coronary artery disease, and heart valve disorders, with age and obesity being significant risk factors. Tachyarrhythmia, a broader category of fast heart rhythms including atrial fibrillation, often arises from conditions such as hyperthyroidism, electrolyte imbalances, and stimulant use, with risk factors including chronic lung disease and excessive alcohol consumption. Both conditions share overlapping causes but differ in their specific triggers and underlying cardiac pathology.
Clinical Presentations Compared
Atrial fibrillation (AF) is characterized by irregularly irregular pulse and absence of distinct P waves on ECG, often presenting with palpitations, fatigue, or shortness of breath. Tachyarrhythmia, encompassing various rapid heart rhythms such as supraventricular tachycardia (SVT) and ventricular tachycardia (VT), typically manifests with sudden onset palpitations, dizziness, or syncope. Differentiating AF from other tachyarrhythmias relies on specific ECG findings and symptom patterns, which guide targeted clinical management and treatment strategies.
Diagnostic Criteria and Tools
Atrial fibrillation is diagnosed primarily through electrocardiogram (ECG) showing irregularly irregular R-R intervals and absence of distinct P waves, whereas tachyarrhythmia encompasses various fast heart rhythms requiring identification of underlying rhythm on ECG. Holter monitoring and event recorders provide continuous rhythm assessment essential for detecting intermittent episodes of atrial fibrillation and tachyarrhythmias. Advanced diagnostics such as electrophysiological studies and cardiac MRI aid in characterizing structural abnormalities contributing to complex tachyarrhythmias versus isolated atrial fibrillation.
Impact on Cardiovascular Health
Atrial fibrillation (AF) and tachyarrhythmia both disrupt normal heart rhythm but affect cardiovascular health differently; AF causes irregular and often rapid heartbeats leading to increased risk of stroke and heart failure, while tachyarrhythmia refers to various fast heart rhythms that can reduce cardiac output and trigger myocardial ischemia. AF increases susceptibility to thromboembolic events due to stasis of blood in the atria, whereas sustained tachyarrhythmia can cause arrhythmia-induced cardiomyopathy and exacerbate existing cardiovascular conditions. Effective management of AF and tachyarrhythmia is crucial to minimize adverse outcomes such as sudden cardiac arrest and progressively impaired ventricular function.
Treatment Approaches and Management Strategies
Effective treatment approaches for atrial fibrillation (AFib) primarily involve rate control using beta-blockers, calcium channel blockers, or digoxin, rhythm control with antiarrhythmic drugs such as amiodarone or flecainide, and anticoagulation therapy to reduce stroke risk with agents like warfarin or direct oral anticoagulants (DOACs). Tachyarrhythmias, including supraventricular and ventricular tachycardia, require tailored management through vagal maneuvers, administration of adenosine for supraventricular tachycardias, or synchronized cardioversion in unstable patients, alongside antiarrhythmics or catheter ablation in refractory cases. Continuous monitoring, lifestyle modification, and addressing underlying conditions contribute to long-term management and prevention of recurrence in both disorders.
Complications and Prognosis
Atrial fibrillation (AFib) significantly increases the risk of stroke, heart failure, and thromboembolism due to irregular atrial contractions leading to blood stasis. Tachyarrhythmia, encompassing rapid heart rhythms like ventricular tachycardia, can result in hemodynamic instability, sudden cardiac arrest, and myocardial ischemia if untreated. Prognosis varies with underlying conditions, but AFib generally poses chronic management challenges and stroke prevention, whereas tachyarrhythmia often requires urgent intervention to prevent fatal outcomes.
Preventive Measures and Lifestyle Modifications
Preventive measures for atrial fibrillation (AFib) and tachyarrhythmia emphasize controlling risk factors such as hypertension, obesity, and diabetes through regular medical check-ups and medication adherence. Lifestyle modifications include maintaining a heart-healthy diet, engaging in consistent aerobic exercise, limiting alcohol intake, and avoiding excessive caffeine and tobacco use to reduce arrhythmia triggers. Stress management techniques like mindfulness and adequate sleep contribute to lowering the incidence and severity of both AFib and tachyarrhythmias.
Future Directions in Research and Therapy
Emerging research in atrial fibrillation (AF) and tachyarrhythmia emphasizes precision medicine approaches, including genetic profiling and advanced imaging techniques to improve arrhythmia detection and individualized therapy. Innovations in catheter ablation technology and development of targeted antiarrhythmic drugs aim to enhance efficacy while minimizing side effects. Ongoing clinical trials investigate novel biomarkers and gene editing strategies to prevent arrhythmia progression and reduce associated stroke risk.
Atrial fibrillation Infographic
 libterm.com
libterm.com