Dermatofibroma is a common benign skin growth that often appears as a small, firm nodule, usually on the arms or legs. These lesions are typically harmless but can sometimes cause discomfort or concern due to their appearance. Discover more about dermatofibroma symptoms, treatment options, and when to seek medical advice in the rest of the article.
Table of Comparison
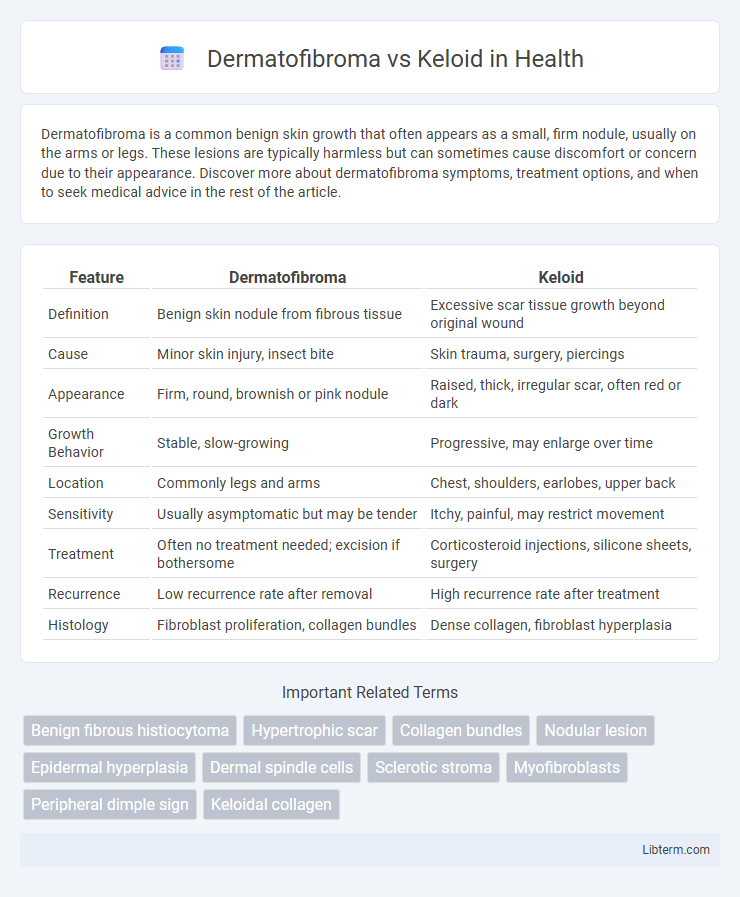
| Feature | Dermatofibroma | Keloid |
|---|---|---|
| Definition | Benign skin nodule from fibrous tissue | Excessive scar tissue growth beyond original wound |
| Cause | Minor skin injury, insect bite | Skin trauma, surgery, piercings |
| Appearance | Firm, round, brownish or pink nodule | Raised, thick, irregular scar, often red or dark |
| Growth Behavior | Stable, slow-growing | Progressive, may enlarge over time |
| Location | Commonly legs and arms | Chest, shoulders, earlobes, upper back |
| Sensitivity | Usually asymptomatic but may be tender | Itchy, painful, may restrict movement |
| Treatment | Often no treatment needed; excision if bothersome | Corticosteroid injections, silicone sheets, surgery |
| Recurrence | Low recurrence rate after removal | High recurrence rate after treatment |
| Histology | Fibroblast proliferation, collagen bundles | Dense collagen, fibroblast hyperplasia |
Introduction to Dermatofibroma and Keloid
Dermatofibroma is a common benign skin nodule typically arising from fibroblasts and histiocytes, often presenting as a firm, hyperpigmented lesion primarily on the extremities. Keloids are raised, irregular scars caused by excessive collagen deposition during wound healing, extending beyond the original injury margin and frequently developing on the chest, shoulders, and earlobes. Differentiating these lesions is crucial due to their distinct pathophysiology, clinical appearance, and treatment approaches.
Key Differences in Definition
Dermatofibroma is a benign skin growth characterized by a firm, raised nodule, typically resulting from minor skin trauma or insect bites. Keloid is an overgrowth of dense fibrous tissue that extends beyond the original wound boundaries due to abnormal collagen production during the healing process. Unlike dermatofibromas, keloids often appear shiny, reddish, and continue to grow over time, causing cosmetic concerns and potential discomfort.
Causes and Risk Factors
Dermatofibromas develop due to minor skin injuries like insect bites or trauma, with risk factors including middle-aged adults and females being more predisposed. Keloids arise from an overgrowth of scar tissue following skin wounds, often linked to genetic predisposition, darker skin tones, and areas subject to tension or repeated injury. Both conditions are influenced by individual healing responses, but keloids tend to extend beyond the original injury site contrary to dermatofibromas.
Clinical Presentation and Appearance
Dermatofibromas typically present as firm, hyperpigmented nodules that are usually less than 1 cm in diameter and exhibit a characteristic dimple sign when pinched. Keloids appear as raised, shiny, and smooth overgrowths of scar tissue that extend beyond the original wound margins, often causing pruritus or discomfort. Both lesions differ in color, texture, and growth behavior, with dermatofibromas being stable and keloids prone to progressive enlargement.
Histopathological Features
Dermatofibroma histopathology reveals a well-circumscribed dermal nodule composed of spindle-shaped fibroblasts and collagen bundles with overlying epidermal hyperplasia and basal layer pigmentation. Keloid tissue shows thick, hyalinized, eosinophilic collagen bundles arranged haphazardly in the dermis with an absence of a sharp border, often extending beyond the original wound margins. Immunohistochemically, dermatofibromas express factor XIIIa and CD34 negativity, while keloids display increased myofibroblast proliferation marked by alpha-smooth muscle actin (a-SMA).
Common Sites of Occurrence
Dermatofibromas commonly occur on the lower legs, particularly the shins, while keloids frequently develop on the chest, shoulders, earlobes, and upper back. Both lesions can arise at sites of skin injury, but keloids are more prone to form in areas with increased skin tension or trauma. Understanding the typical locations aids in differentiating between benign fibrous growths and pathological scar tissue.
Diagnosis and Differentiation
Dermatofibomas present as firm, hyperpigmented nodules often found on extremities, diagnosed through clinical examination and confirmed by histopathology showing spindle-shaped fibroblasts and collagen bundles. Keloids are raised, thickened scars extending beyond the original wound edges, diagnosed by their characteristic history of trauma and biopsy revealing excessive collagen deposition with disorganized bundles. Differentiating factors include the growth pattern, with dermatofibromas being stable or slowly growing localized lesions, whereas keloids exhibit aggressive expansion and do not regress spontaneously.
Treatment Options for Each Condition
Treatment of dermatofibroma typically involves conservative management, with surgical excision reserved for symptomatic or cosmetically concerning lesions, while cryotherapy and corticosteroid injections may reduce lesion size. Keloid treatment emphasizes prevention and includes options like intralesional corticosteroids, silicone gel sheets, laser therapy, and surgical excision combined with adjuvant therapies to minimize recurrence. Emerging treatments for keloids also explore radiotherapy and novel molecular therapies targeting fibrosis pathways, reflecting a more aggressive approach compared to dermatofibroma management.
Prognosis and Recurrence Rates
Dermatofibromas have an excellent prognosis with rare recurrence after simple excision, typically presenting as benign, stable nodules. Keloids exhibit a higher recurrence rate, ranging from 40% to 70%, due to aggressive fibroblast proliferation and collagen deposition beyond the original wound margin. Effective treatment of keloids involves multimodal approaches including corticosteroid injections, laser therapy, or surgery combined with adjuvants to minimize recurrence.
Prevention and Patient Education
Preventing dermatofibromas and keloids involves minimizing skin trauma such as cuts, insect bites, or injections, especially in individuals with a genetic predisposition to keloid formation. Patient education emphasizes proper wound care, avoiding unnecessary skin punctures, and seeking early treatment to reduce excessive scar tissue development. Regular monitoring by dermatologists can help manage symptoms and prevent progression of both dermatofibromas and keloids.
Dermatofibroma Infographic
 libterm.com
libterm.com