Corneal ulcers are open sores on the cornea, often caused by infections, trauma, or underlying eye conditions, leading to redness, pain, and vision impairment. Prompt diagnosis and treatment are essential to prevent complications such as scarring or vision loss. Discover effective prevention methods and treatment options to protect your eye health throughout this article.
Table of Comparison
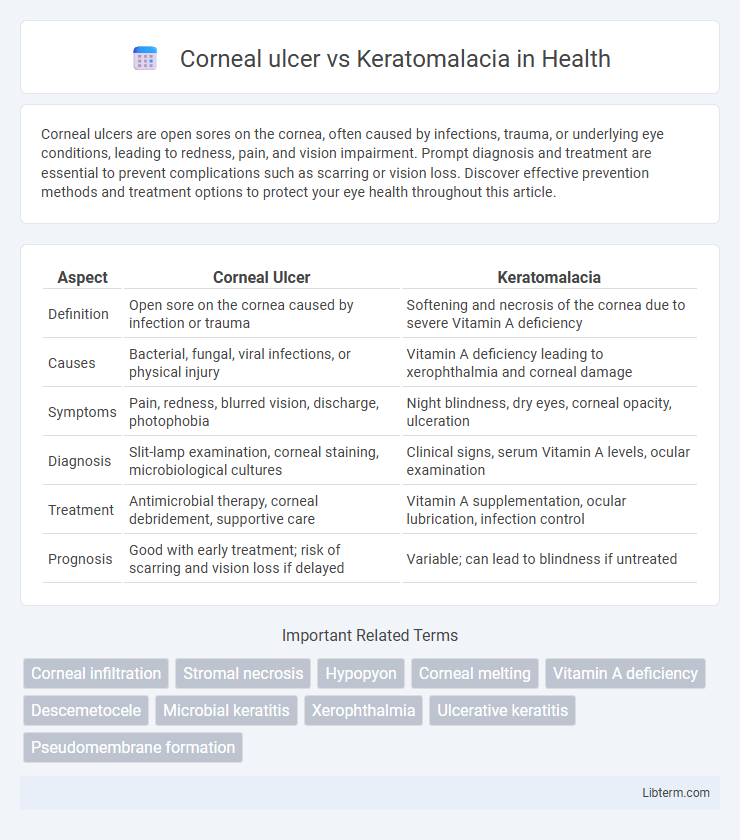
| Aspect | Corneal Ulcer | Keratomalacia |
|---|---|---|
| Definition | Open sore on the cornea caused by infection or trauma | Softening and necrosis of the cornea due to severe Vitamin A deficiency |
| Causes | Bacterial, fungal, viral infections, or physical injury | Vitamin A deficiency leading to xerophthalmia and corneal damage |
| Symptoms | Pain, redness, blurred vision, discharge, photophobia | Night blindness, dry eyes, corneal opacity, ulceration |
| Diagnosis | Slit-lamp examination, corneal staining, microbiological cultures | Clinical signs, serum Vitamin A levels, ocular examination |
| Treatment | Antimicrobial therapy, corneal debridement, supportive care | Vitamin A supplementation, ocular lubrication, infection control |
| Prognosis | Good with early treatment; risk of scarring and vision loss if delayed | Variable; can lead to blindness if untreated |
Introduction to Corneal Ulcer and Keratomalacia
Corneal ulcer is an open sore on the cornea caused by infections, trauma, or dry eye, often leading to pain, redness, and vision loss if untreated. Keratomalacia results from severe vitamin A deficiency, causing corneal dryness, softening, and potential corneal melting, predominantly affecting malnourished populations. Both conditions threaten corneal integrity but differ in etiology and pathophysiology, requiring distinct diagnostic and treatment approaches.
Definition and Overview
Corneal ulcer is an open sore on the cornea caused by infections, trauma, or dry eye, leading to pain, redness, and vision impairment. Keratomalacia is a severe eye disorder resulting from vitamin A deficiency, characterized by corneal softening and necrosis that can lead to blindness. Both conditions affect the cornea but differ in etiology, with corneal ulcer linked to infectious or mechanical damage and keratomalacia associated with nutritional deficiency.
Epidemiology and Risk Factors
Corneal ulcer primarily affects individuals in developing countries with poor access to eye care, often linked to trauma, contact lens use, or bacterial, fungal, or viral infections. Keratomalacia, caused by severe vitamin A deficiency, predominantly occurs in malnourished children under five in low-income regions, especially in sub-Saharan Africa and South Asia. Risk factors for corneal ulcer include ocular surface damage and immunosuppression, while keratomalacia risk factors are closely tied to malnutrition, measles, and inadequate vitamin A intake.
Etiology and Causes
Corneal ulcer primarily results from bacterial, fungal, or viral infections following ocular trauma, contact lens misuse, or dry eye syndrome, leading to epithelial loss and stromal inflammation. Keratomalacia develops due to severe vitamin A deficiency, causing corneal epithelial degeneration and liquefactive necrosis, predominantly in malnourished populations. Both conditions involve corneal damage but differ fundamentally in infectious versus nutritional etiologies.
Clinical Features and Symptoms
Corneal ulcer presents with severe eye pain, redness, photophobia, discharge, and decreased vision, often accompanied by a visible white or grayish infiltrate on the cornea. Keratomalacia is characterized by rapid corneal melting and liquefaction due to severe vitamin A deficiency, leading to soft, necrotic corneal tissue, marked xerosis, and night blindness preceding ulceration. Both conditions cause visual impairment, but keratomalacia is distinct with systemic signs of malnutrition and ocular surface dryness.
Diagnostic Approaches
Corneal ulcer diagnosis relies on slit-lamp biomicroscopy to identify epithelial defects and stromal infiltration, often aided by fluorescein staining to highlight ulcerated areas. Keratomalacia, primarily linked to severe vitamin A deficiency, is diagnosed through clinical signs such as corneal softening and melting, with serum retinol levels serving as a critical biochemical marker. Microbiological cultures and vitamin A assays are essential for distinguishing infectious keratitis in corneal ulcer from nutritional causes in keratomalacia.
Pathophysiological Differences
Corneal ulcer involves a localized epithelial defect with stromal inflammation primarily caused by bacterial, viral, or fungal infections leading to extracellular matrix degradation and neutrophil infiltration. Keratomalacia results from severe vitamin A deficiency causing liquefactive necrosis of the corneal stroma, epithelial keratinization, and widespread stromal melting due to disrupted epithelial integrity and impaired mucin production. The key pathophysiological difference lies in infection-driven inflammatory destruction in corneal ulcer versus metabolic and nutritional-induced stromal necrosis in keratomalacia.
Treatment Modalities
Corneal ulcer treatment includes topical antibiotics, antifungals, or antivirals based on the infectious agent, with adjunctive therapies such as cycloplegics and corticosteroids used cautiously. Keratomalacia requires aggressive vitamin A supplementation, both orally and topically, to reverse corneal melting and prevent blindness, alongside supportive measures like lubricating eye drops. Early diagnosis and tailored treatment in both conditions are critical to preserving vision and preventing permanent corneal damage.
Prognosis and Complications
Corneal ulcers typically have a favorable prognosis with prompt antibiotic treatment but can lead to serious complications such as corneal scarring, vision loss, or perforation if untreated. Keratomalacia, caused by severe vitamin A deficiency, often results in rapid corneal melting and extensive ulceration, leading to irreversible blindness and higher mortality rates without aggressive nutritional and medical intervention. Both conditions require immediate diagnosis and management to prevent long-term ocular morbidity and systemic complications.
Prevention and Public Health Strategies
Effective prevention of corneal ulcer and keratomalacia hinges on improving ocular hygiene, prompt treatment of ocular infections, and addressing vitamin A deficiency at the community level. Public health strategies emphasize mass vitamin A supplementation, nutritional education, and access to clean water to reduce keratomalacia risk, particularly in children. For corneal ulcers, early detection through community eye screening programs and provision of affordable antibiotics are crucial to prevent severe vision loss.
Corneal ulcer Infographic
 libterm.com
libterm.com