A fistula is an abnormal connection between two body parts, such as organs or blood vessels, often resulting from injury, infection, or surgery. These connections can cause complications like infection or impaired organ function, requiring medical diagnosis and treatment. Explore this article to understand the types, causes, symptoms, and treatment options for fistulas to better manage Your health.
Table of Comparison
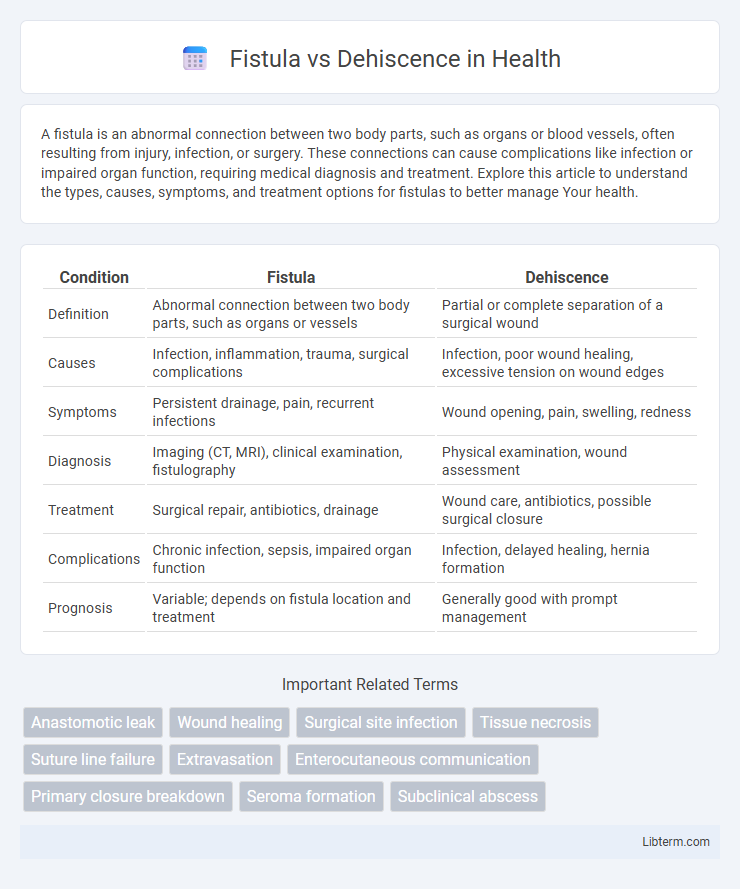
| Condition | Fistula | Dehiscence |
|---|---|---|
| Definition | Abnormal connection between two body parts, such as organs or vessels | Partial or complete separation of a surgical wound |
| Causes | Infection, inflammation, trauma, surgical complications | Infection, poor wound healing, excessive tension on wound edges |
| Symptoms | Persistent drainage, pain, recurrent infections | Wound opening, pain, swelling, redness |
| Diagnosis | Imaging (CT, MRI), clinical examination, fistulography | Physical examination, wound assessment |
| Treatment | Surgical repair, antibiotics, drainage | Wound care, antibiotics, possible surgical closure |
| Complications | Chronic infection, sepsis, impaired organ function | Infection, delayed healing, hernia formation |
| Prognosis | Variable; depends on fistula location and treatment | Generally good with prompt management |
Introduction to Fistula and Dehiscence
Fistula is an abnormal connection between two epithelialized surfaces, often resulting from infection, inflammation, or surgical complications. Dehiscence refers to the partial or complete separation of a surgical wound or incision, typically caused by poor healing, infection, or mechanical stress. Both conditions impair tissue integrity and require prompt medical evaluation to prevent complications.
Definitions: Fistula vs Dehiscence
Fistula is an abnormal connection between two epithelialized surfaces, often resulting from infection, surgery, or inflammation, creating a passage that enables fluid or air to bypass normal anatomical routes. Dehiscence refers to the partial or complete separation of a surgical wound or incision along its sutures, exposing underlying tissues and potentially leading to infection or delayed healing. Both conditions represent postoperative complications but differ fundamentally in their definition, with fistula involving abnormal tract formation and dehiscence involving wound disruption.
Causes and Risk Factors
Fistulas commonly develop due to chronic infections, inflammation, or surgical complications causing abnormal connections between organs or tissues. Dehiscence occurs primarily from wound healing failure, often linked to factors such as poor surgical technique, infection, malnutrition, or increased intra-abdominal pressure. Both conditions share risk factors like diabetes, immunosuppression, and obesity, which impair tissue repair and promote complications.
Clinical Presentation and Symptoms
Fistula commonly presents with abnormal drainage of fluid or pus from an opening on the skin or mucosal surface, often accompanied by localized pain, swelling, and recurrent infections. Dehiscence is characterized by the partial or complete separation of a surgical incision, resulting in evident wound opening, increased discharge, redness, and tenderness around the incision site. Both conditions may present with fever and systemic signs of infection depending on severity, necessitating prompt clinical evaluation and treatment.
Pathophysiology: Understanding the Differences
Fistula and dehiscence differ fundamentally in pathophysiology, as a fistula involves the abnormal connection between two epithelialized surfaces due to chronic inflammation or infection, leading to persistent drainage and communication. Dehiscence refers to the partial or complete separation of a surgical wound caused by mechanical stress, impaired healing, or increased intra-abdominal pressure, resulting in wound disruption. Understanding these mechanisms aids in targeted treatment strategies to promote healing and prevent complications.
Diagnostic Approaches
Diagnostic approaches for fistula primarily involve imaging techniques like contrast-enhanced CT scans, MRI, and fistulography to visualize abnormal connections between organs or tissues. Dehiscence diagnosis relies on physical examination for wound separation, ultrasound to assess fluid collections, and sometimes CT imaging to evaluate deeper fascial disruptions. Both conditions benefit from laboratory tests to identify infection markers and guide treatment planning.
Treatment and Management Options
Treatment of fistula typically involves conservative management with antibiotics, drainage, and sometimes surgical intervention such as fistulectomy or seton placement to promote healing and prevent infection. Dehiscence management depends on the extent of wound separation, ranging from wound care with dressings and negative pressure wound therapy to surgical re-closure or flap reconstruction for severe cases. Both conditions require careful monitoring for infection, appropriate use of imaging modalities, and patient-specific strategies to optimize healing outcomes.
Prognosis and Complications
Fistula often results in chronic infection and persistent drainage, leading to prolonged healing times and potential systemic complications such as sepsis if untreated. Dehiscence primarily increases the risk of wound infection, abscess formation, and delayed tissue regeneration, which may require surgical intervention to prevent further morbidity. Prognosis for fistula is generally guarded due to complex anatomy and risk of recurrence, whereas dehiscence prognosis improves significantly with prompt wound management and stabilization.
Prevention Strategies
Effective prevention strategies for fistula and dehiscence focus on meticulous surgical technique and optimal wound care. Maintaining sterile conditions, ensuring proper tissue handling, and adequate blood supply reduce the risk of tissue breakdown. Postoperative monitoring for early signs of infection or stress on the wound site is crucial to prevent complications and promote healing.
Key Takeaways and Summary
Fistula refers to an abnormal connection between two body parts, often causing persistent drainage, while dehiscence is the reopening or separation of a surgical wound, potentially exposing underlying tissues. Key takeaways include recognizing fistula by continuous discharge and abnormal pathways, whereas dehiscence presents with wound separation and risk of infection or delayed healing. Effective management requires accurate diagnosis to address fistula with drainage control and possible surgical repair, and dehiscence through wound closure and infection prevention strategies.
Fistula Infographic
 libterm.com
libterm.com