Gastroesophageal Reflux Disease (GERD) causes stomach acid to flow back into the esophagus, leading to symptoms like heartburn, chest discomfort, and difficulty swallowing. Understanding the triggers and treatment options can help you manage this chronic condition effectively. Explore the article further to learn how to alleviate your symptoms and improve your quality of life.
Table of Comparison
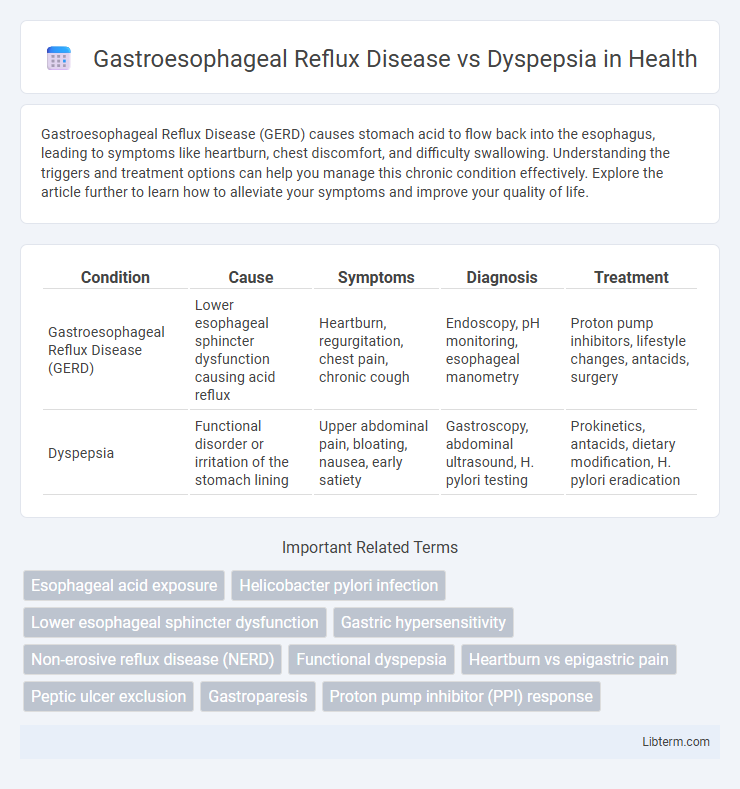
| Condition | Cause | Symptoms | Diagnosis | Treatment |
|---|---|---|---|---|
| Gastroesophageal Reflux Disease (GERD) | Lower esophageal sphincter dysfunction causing acid reflux | Heartburn, regurgitation, chest pain, chronic cough | Endoscopy, pH monitoring, esophageal manometry | Proton pump inhibitors, lifestyle changes, antacids, surgery |
| Dyspepsia | Functional disorder or irritation of the stomach lining | Upper abdominal pain, bloating, nausea, early satiety | Gastroscopy, abdominal ultrasound, H. pylori testing | Prokinetics, antacids, dietary modification, H. pylori eradication |
Understanding Gastroesophageal Reflux Disease (GERD)
Gastroesophageal Reflux Disease (GERD) is a chronic condition characterized by the backflow of stomach acid into the esophagus, causing symptoms such as heartburn, regurgitation, and chest pain. Unlike dyspepsia, which primarily involves upper abdominal discomfort and bloating without reflux, GERD results from the malfunction of the lower esophageal sphincter allowing acid to irritate the esophageal lining. Effective diagnosis of GERD often involves endoscopy, pH monitoring, and symptom assessment to distinguish it from other gastrointestinal disorders like dyspepsia.
What Is Dyspepsia?
Dyspepsia, commonly known as indigestion, refers to a group of symptoms including upper abdominal discomfort, bloating, nausea, and early satiety, often without an identifiable organic cause. Unlike Gastroesophageal Reflux Disease (GERD), which primarily involves the reflux of stomach acid into the esophagus causing heartburn and acid regurgitation, dyspepsia is associated with impaired gastric motility or hypersensitivity of the stomach lining. Effective diagnosis of dyspepsia relies on symptom assessment and exclusion of other gastrointestinal conditions, often requiring endoscopy when alarm features are present.
Key Symptoms: GERD vs Dyspepsia
Gastroesophageal Reflux Disease (GERD) is primarily characterized by heartburn, acid regurgitation, and chest discomfort due to the backflow of stomach acid into the esophagus. Dyspepsia, also known as indigestion, commonly presents with symptoms such as upper abdominal bloating, nausea, early satiety, and epigastric pain without the pronounced acid reflux seen in GERD. Differentiating GERD from dyspepsia relies on identifying the dominant presence of acid-related symptoms in GERD compared to the broader spectrum of vague upper gastrointestinal discomfort typical of dyspepsia.
Common Causes and Triggers
Gastroesophageal Reflux Disease (GERD) commonly results from lower esophageal sphincter dysfunction, leading to acid reflux, with triggers including fatty foods, caffeine, alcohol, and obesity. Dyspepsia, often caused by Helicobacter pylori infection, delayed gastric emptying, or functional disorders, is typically triggered by large meals, spicy foods, and stress. Both conditions share dietary and lifestyle factors but differ in underlying pathophysiology and symptom presentation.
Diagnostic Differences: GERD and Dyspepsia
Gastroesophageal Reflux Disease (GERD) is primarily diagnosed through clinical evaluation of symptoms such as heartburn and acid regurgitation, often supported by esophageal pH monitoring and endoscopy to assess mucosal damage. Dyspepsia, characterized by upper abdominal discomfort and bloating, requires exclusion of organic causes via upper endoscopy and may involve tests for Helicobacter pylori infection. Unlike GERD, dyspepsia diagnosis focuses on symptom patterns and ruling out peptic ulcer disease, malignancy, and motility disorders.
Risk Factors for GERD and Dyspepsia
Gastroesophageal Reflux Disease (GERD) risk factors include obesity, hiatal hernia, pregnancy, smoking, and dietary triggers such as fatty or spicy foods, which contribute to lower esophageal sphincter dysfunction. Dyspepsia risk factors encompass Helicobacter pylori infection, use of nonsteroidal anti-inflammatory drugs (NSAIDs), stress, and functional gastrointestinal disorders, often without structural abnormalities. Both conditions share overlapping symptoms but differ significantly in underlying causes and risk profiles.
Treatment Options for GERD
Treatment options for Gastroesophageal Reflux Disease (GERD) primarily include lifestyle modifications such as weight loss, dietary changes, and elevating the head during sleep. Pharmacological therapies involve proton pump inhibitors (PPIs), H2 receptor blockers, and antacids to reduce gastric acid production and alleviate symptoms. In severe or refractory cases, surgical interventions like Nissen fundoplication or endoscopic procedures may be considered to enhance lower esophageal sphincter function.
Managing Dyspepsia: Approaches and Therapies
Managing dyspepsia involves a combination of lifestyle modifications such as dietary changes, stress management, and avoiding trigger foods along with pharmacological treatments including proton pump inhibitors, H2-receptor antagonists, and prokinetics. Identifying whether symptoms stem from functional dyspepsia or an organic cause is crucial for targeted therapy and improving patient outcomes. Regular monitoring and tailored treatment plans help differentiate managing dyspepsia from gastroesophageal reflux disease, which often requires different therapeutic strategies focused on acid suppression and barrier enhancement.
Lifestyle Modifications for Symptom Relief
Lifestyle modifications for Gastroesophageal Reflux Disease (GERD) include avoiding trigger foods such as spicy and fatty meals, maintaining a healthy weight, elevating the head during sleep, and refraining from lying down immediately after eating to reduce acid reflux. In cases of dyspepsia, symptom relief often involves eating smaller, more frequent meals, reducing alcohol and caffeine intake, and managing stress through relaxation techniques. Both conditions benefit significantly from quitting smoking and incorporating regular, moderate exercise to improve digestive health and minimize discomfort.
When to Seek Medical Advice
Persistent heartburn and acid regurgitation occurring more than twice a week often indicate Gastroesophageal Reflux Disease (GERD) and require medical evaluation to prevent complications such as esophagitis or Barrett's esophagus. Dyspepsia symptoms like upper abdominal pain, bloating, and early satiety that persist or worsen, especially when accompanied by weight loss, vomiting, or anemia, warrant prompt consultation for potential underlying causes such as peptic ulcer or malignancy. Seeking medical advice is crucial when over-the-counter medications fail to relieve symptoms or when alarming signs emerge, as timely diagnosis improves management outcomes in both GERD and dyspepsia.
Gastroesophageal Reflux Disease Infographic
 libterm.com
libterm.com