Hyperpnea is characterized by an increased depth and rate of breathing, often occurring in response to higher oxygen demand or metabolic activity. This physiological response can be triggered by exercise, fever, or certain medical conditions, leading to enhanced ventilation and improved gas exchange. Discover how hyperpnea affects your respiratory system and when it may signal underlying health issues by reading the rest of the article.
Table of Comparison
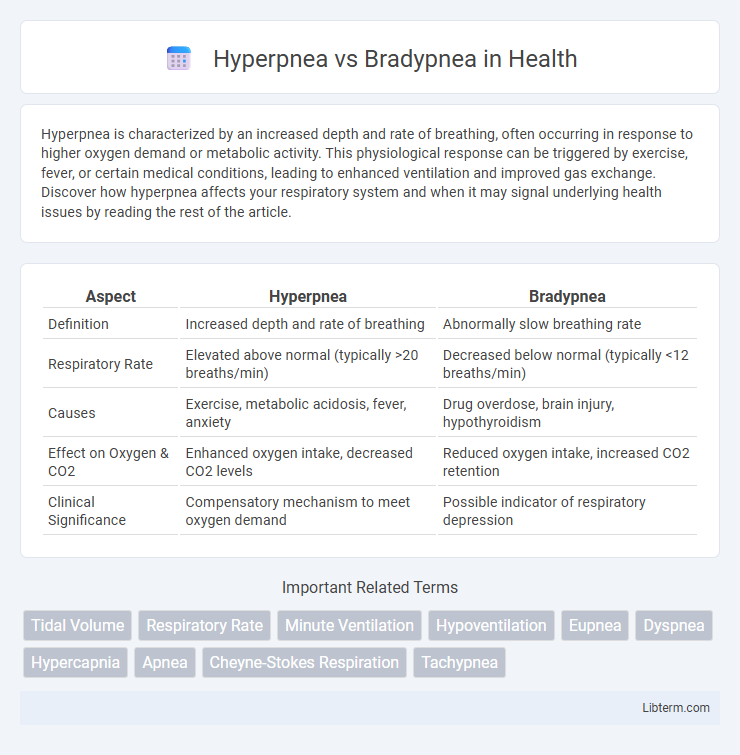
| Aspect | Hyperpnea | Bradypnea |
|---|---|---|
| Definition | Increased depth and rate of breathing | Abnormally slow breathing rate |
| Respiratory Rate | Elevated above normal (typically >20 breaths/min) | Decreased below normal (typically <12 breaths/min) |
| Causes | Exercise, metabolic acidosis, fever, anxiety | Drug overdose, brain injury, hypothyroidism |
| Effect on Oxygen & CO2 | Enhanced oxygen intake, decreased CO2 levels | Reduced oxygen intake, increased CO2 retention |
| Clinical Significance | Compensatory mechanism to meet oxygen demand | Possible indicator of respiratory depression |
Understanding Breathing Patterns: Hyperpnea and Bradypnea
Hyperpnea refers to an increased depth and rate of breathing often triggered by physical exertion or metabolic acidosis, enhancing oxygen intake and carbon dioxide removal. Bradypnea is characterized by abnormally slow breathing, typically below 12 breaths per minute, and may result from neurological disorders, drug overdose, or hypothyroidism. Differentiating these respiratory patterns is essential in clinical diagnosis to assess underlying conditions affecting respiratory efficiency.
What is Hyperpnea? Definition and Causes
Hyperpnea is characterized by an increased depth and rate of breathing, often occurring in response to heightened metabolic demand such as exercise, high altitude, or fever. This respiratory pattern ensures enhanced oxygen intake and carbon dioxide removal to meet the body's elevated oxygen requirements. Common causes of hyperpnea include strenuous physical activity, metabolic acidosis, sepsis, and certain neurological conditions that stimulate breathing centers.
What is Bradypnea? Definition and Causes
Bradypnea is a clinical condition characterized by an abnormally slow respiratory rate, typically fewer than 12 breaths per minute in adults. Causes of bradypnea include drug overdose (especially opioids or sedatives), hypothyroidism, elevated intracranial pressure, and certain neurological disorders such as encephalitis or brain injury. Unlike hyperpnea, which involves increased depth and rate of breathing, bradypnea reflects reduced respiratory frequency that may lead to inadequate oxygen intake and increased carbon dioxide retention.
Key Differences Between Hyperpnea and Bradypnea
Hyperpnea is characterized by an increased depth and rate of breathing, often in response to metabolic demands like exercise or acidosis, while bradypnea refers to abnormally slow breathing rates, typically below 12 breaths per minute in adults, which can result from central nervous system depression or metabolic imbalances. Hyperpnea involves active respiration with adequate oxygenation and carbon dioxide removal, whereas bradypnea can cause hypoventilation, leading to elevated carbon dioxide levels and respiratory acidosis. The key diagnostic distinction lies in respiratory rate measurement and clinical context, with hyperpnea indicating compensatory hyperventilation and bradypnea signaling potentially pathological respiratory depression.
Signs and Symptoms of Hyperpnea
Hyperpnea is characterized by an increased depth and rate of breathing, often seen during exercise, metabolic acidosis, or hypoxia, presenting with rapid, deep breaths that enhance oxygen intake and carbon dioxide elimination. Signs and symptoms include noticeable labored breathing, shortness of breath, and sometimes a feeling of air hunger. Bradypnea, in contrast, is identified by abnormally slow breathing rates, which may lead to inadequate ventilation and symptoms like dizziness, fatigue, or confusion due to insufficient oxygen delivery.
Signs and Symptoms of Bradypnea
Bradypnea is characterized by an abnormally slow respiratory rate, typically fewer than 12 breaths per minute in adults, often presenting with signs such as fatigue, dizziness, and confusion due to inadequate oxygen intake. Patients may experience shortness of breath, chest pain, or cyanosis when oxygen levels drop significantly. In contrast, hyperpnea involves deep and rapid breathing, usually as a response to increased metabolic demand or respiratory distress.
Medical Conditions Linked to Hyperpnea
Hyperpnea is characterized by abnormally deep or rapid breathing often linked to medical conditions such as metabolic acidosis, sepsis, and heart failure, where the body attempts to compensate for oxygen deficiency or increased carbon dioxide levels. Bradypnea, in contrast, involves abnormally slow breathing rates commonly associated with conditions like hypothyroidism, brain injury, or opioid overdose. Understanding these respiratory patterns is critical in diagnosing underlying disorders and managing patients with respiratory or systemic illnesses.
Medical Conditions Linked to Bradypnea
Bradypnea, characterized by abnormally slow breathing rates below 12 breaths per minute in adults, is commonly linked to medical conditions such as hypothyroidism, severe brain injury, and drug overdose, particularly opioids and sedatives. Unlike hyperpnea, which involves increased depth and rate of breathing often seen in metabolic acidosis or exercise, bradypnea signals impaired respiratory drive or neuromuscular dysfunction. Accurate diagnosis requires monitoring respiratory patterns alongside underlying pathologies to ensure appropriate treatment.
Diagnosis: How Hyperpnea and Bradypnea Are Identified
Hyperpnea is identified through clinical observation of increased depth and rate of breathing, often confirmed by arterial blood gas analysis showing reduced carbon dioxide levels and increased oxygen intake. Bradypnea diagnosis relies on detecting abnormally slow respiratory rates via physical examination and monitoring devices like pulse oximeters and capnography, with potential underlying causes revealed through neurological and metabolic assessments. Both conditions require correlating respiratory patterns with patient history and diagnostic imaging to determine etiology and guide treatment.
Treatment and Management for Abnormal Breathing Patterns
Treatment of hyperpnea involves addressing underlying causes such as metabolic acidosis or hypoxia, often through supplemental oxygen or ventilation support to normalize respiratory rate and depth. Management of bradypnea includes monitoring for potential causes like drug overdose or neurological disorders, with interventions such as naloxone administration or mechanical ventilation when necessary. Both abnormal breathing patterns require continuous assessment and supportive care tailored to the patient's specific etiology and clinical status.
Hyperpnea Infographic
 libterm.com
libterm.com