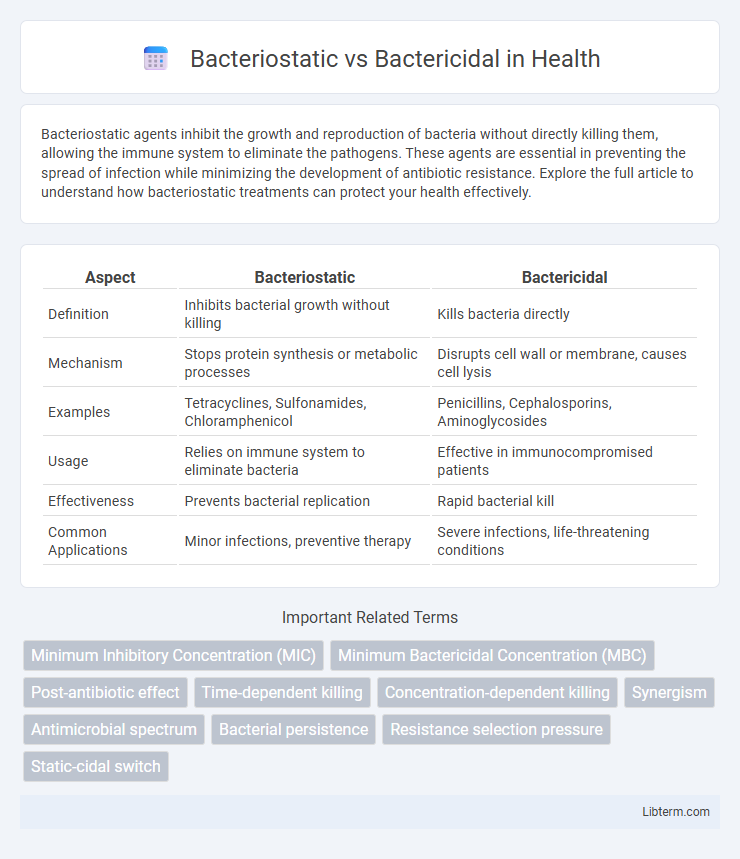
Bacteriostatic agents inhibit the growth and reproduction of bacteria without directly killing them, allowing the immune system to eliminate the pathogens. These agents are essential in preventing the spread of infection while minimizing the development of antibiotic resistance. Explore the full article to understand how bacteriostatic treatments can protect your health effectively.
Table of Comparison
| Aspect | Bacteriostatic | Bactericidal |
|---|---|---|
| Definition | Inhibits bacterial growth without killing | Kills bacteria directly |
| Mechanism | Stops protein synthesis or metabolic processes | Disrupts cell wall or membrane, causes cell lysis |
| Examples | Tetracyclines, Sulfonamides, Chloramphenicol | Penicillins, Cephalosporins, Aminoglycosides |
| Usage | Relies on immune system to eliminate bacteria | Effective in immunocompromised patients |
| Effectiveness | Prevents bacterial replication | Rapid bacterial kill |
| Common Applications | Minor infections, preventive therapy | Severe infections, life-threatening conditions |
Introduction to Antibacterial Agents
Antibacterial agents are classified as bacteriostatic or bactericidal based on their mechanism of action against bacteria. Bacteriostatic agents inhibit bacterial growth and reproduction, relying on the host's immune system to eliminate the infection. Bactericidal agents, by contrast, kill bacteria directly, making them crucial in treating severe or immunocompromised infections.
Defining Bacteriostatic and Bactericidal
Bacteriostatic agents inhibit the growth and reproduction of bacteria without killing them, allowing the immune system to eliminate the pathogens. Bactericidal agents directly kill bacteria, resulting in a rapid reduction of the bacterial population. Understanding the difference between bacteriostatic and bactericidal is essential for selecting appropriate antimicrobial treatments based on infection severity and patient immune status.
Mechanisms of Bacteriostatic Action
Bacteriostatic antibiotics inhibit bacterial growth by targeting essential processes such as protein synthesis, DNA replication, or metabolic pathways. These agents bind to ribosomes, blocking peptide chain elongation and effectively halting bacterial proliferation without directly killing the cells. This mechanism allows the immune system to eliminate the pathogens while preventing further bacterial population expansion.
Mechanisms of Bactericidal Action
Bactericidal agents kill bacteria by directly targeting essential cellular processes such as cell wall synthesis, protein synthesis, and DNA replication, leading to cell death. Common mechanisms include disruption of peptidoglycan cross-linking via beta-lactams, inhibition of ribosomal function by aminoglycosides, and induction of DNA strand breaks through fluoroquinolones. These mechanisms cause irreversible damage that results in bacterial lysis or apoptosis, distinguishing bactericidal action from bacteriostatic agents that merely inhibit growth.
Key Differences Between Bacteriostatic and Bactericidal
Bacteriostatic agents inhibit bacterial growth and reproduction without killing the cells, allowing the immune system to eliminate the infection, while bactericidal agents actively kill bacteria, leading to a rapid decrease in viable bacterial count. Key differences include their mechanisms of action, with bacteriostatic drugs targeting protein synthesis and metabolic pathways, and bactericidal drugs disrupting cell wall synthesis or DNA replication. The clinical choice depends on infection severity and immune status, as bactericidal agents are preferred in immunocompromised patients or severe infections.
Clinical Applications and Therapeutic Choices
Bacteriostatic agents inhibit bacterial growth, allowing the immune system to eliminate pathogens, making them preferred in infections where preserving host defenses is crucial, such as urinary tract infections and intracellular pathogens. Bactericidal drugs directly kill bacteria, which is essential in severe or life-threatening infections like endocarditis, meningitis, or neutropenic patients where rapid bacterial eradication is necessary. Therapeutic choices depend on infection severity, immune status, and pathogen susceptibility, with combination therapy sometimes employed to maximize efficacy and reduce resistance development.
Factors Influencing Antibiotic Selection
Factors influencing antibiotic selection between bacteriostatic and bactericidal agents include the site and severity of infection, the patient's immune status, and the mechanism of bacterial killing required. Bactericidal antibiotics are preferred in life-threatening infections like endocarditis or meningitis where rapid bacterial eradication is critical, while bacteriostatic agents may be sufficient in less severe infections and rely on host immunity for effective clearance. Pharmacokinetics, antibiotic spectrum, and potential resistance also guide clinicians in choosing the appropriate antibiotic class.
Resistance Implications: Bacteriostatic vs Bactericidal
Bacteriostatic agents inhibit bacterial growth without killing the cells, which may allow surviving pathogens to develop resistance mechanisms over time. Bactericidal agents actively kill bacteria, reducing the bacterial load and potentially lowering the risk of resistance emergence. Resistance implications differ as bacteriostatic drugs often require a functional immune response to clear infections, whereas bactericidal drugs directly reduce viable bacteria, influencing treatment strategies in resistant infections.
Safety Profiles and Side Effects
Bacteriostatic agents inhibit bacterial growth without killing the cells, often resulting in fewer side effects and a lower risk of triggering severe immune responses compared to bactericidal agents, which actively kill bacteria but may cause more rapid bacterial toxin release. Safety profiles of bacteriostatic drugs tend to be preferable in patients with compromised immune systems, as these agents rely on the host's immune system to clear inhibited bacteria. Bactericidal antibiotics, while more aggressive, can lead to increased risks of adverse effects such as nephrotoxicity or ototoxicity depending on the drug class, necessitating careful monitoring during treatment.
Conclusion: Optimizing Antibacterial Therapy
Choosing between bacteriostatic and bactericidal agents depends on the infection type, immune status of the patient, and site of infection to maximize therapeutic outcomes. Bactericidal antibiotics are preferred in severe infections like endocarditis or meningitis, whereas bacteriostatic agents can effectively control less critical infections by inhibiting bacterial growth. Tailoring antibacterial therapy using evidence-based pharmacodynamics and microbiological data enhances treatment efficacy and reduces resistance development.
Bacteriostatic Infographic
 libterm.com
libterm.com