Methemoglobin is a form of hemoglobin in which the iron atom is oxidized, reducing its ability to bind oxygen effectively and impairing oxygen delivery to tissues. High levels of methemoglobin can lead to methemoglobinemia, causing symptoms like cyanosis, fatigue, and shortness of breath. Discover more about causes, symptoms, and treatments of methemoglobinemia in the rest of this article.
Table of Comparison
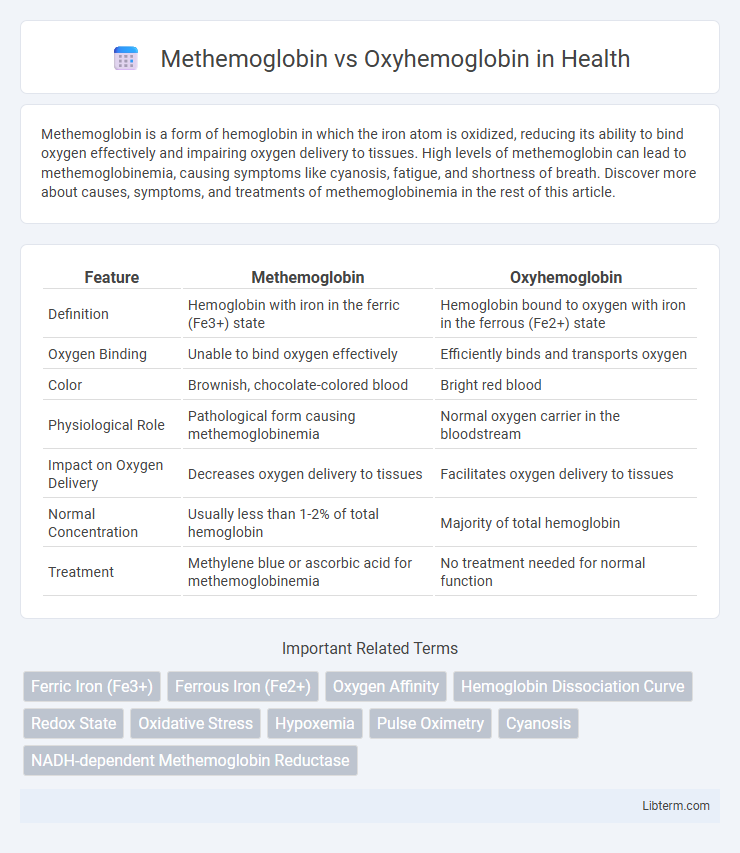
| Feature | Methemoglobin | Oxyhemoglobin |
|---|---|---|
| Definition | Hemoglobin with iron in the ferric (Fe3+) state | Hemoglobin bound to oxygen with iron in the ferrous (Fe2+) state |
| Oxygen Binding | Unable to bind oxygen effectively | Efficiently binds and transports oxygen |
| Color | Brownish, chocolate-colored blood | Bright red blood |
| Physiological Role | Pathological form causing methemoglobinemia | Normal oxygen carrier in the bloodstream |
| Impact on Oxygen Delivery | Decreases oxygen delivery to tissues | Facilitates oxygen delivery to tissues |
| Normal Concentration | Usually less than 1-2% of total hemoglobin | Majority of total hemoglobin |
| Treatment | Methylene blue or ascorbic acid for methemoglobinemia | No treatment needed for normal function |
Introduction to Hemoglobin Variants
Hemoglobin variants such as methemoglobin and oxyhemoglobin differ in their oxygen-binding capabilities and chemical structure. Oxyhemoglobin contains iron in the ferrous (Fe2+) state, enabling efficient oxygen transport and release to tissues, while methemoglobin has iron oxidized to the ferric (Fe3+) state, which cannot bind oxygen effectively. Understanding the balance between these hemoglobin forms is critical for diagnosing and managing disorders related to impaired oxygen delivery.
What is Methemoglobin?
Methemoglobin is a form of hemoglobin in which the iron in the heme group is oxidized from the ferrous (Fe2+) to the ferric (Fe3+) state, rendering it unable to bind oxygen effectively. Unlike oxyhemoglobin, which carries and releases oxygen to tissues, methemoglobin cannot participate in oxygen transport, leading to reduced oxygen delivery and potential hypoxia. Elevated methemoglobin levels, a condition known as methemoglobinemia, impair cellular respiration and may require medical intervention.
What is Oxyhemoglobin?
Oxyhemoglobin is a complex formed when hemoglobin binds to oxygen molecules, enabling efficient oxygen transport from the lungs to tissues. This oxygenated form of hemoglobin facilitates cellular respiration by releasing oxygen where it is needed most. Unlike methemoglobin, which contains oxidized iron and cannot carry oxygen effectively, oxyhemoglobin maintains ferrous iron in hemoglobin, ensuring optimal oxygen delivery throughout the body.
Structural Differences: Methemoglobin vs Oxyhemoglobin
Methemoglobin contains iron in the ferric (Fe3+) state, preventing it from binding oxygen effectively, unlike oxyhemoglobin, which has iron in the ferrous (Fe2+) state enabling reversible oxygen binding. The oxidation of iron in methemoglobin alters the heme group's electronic configuration, distorting the heme pocket and decreasing oxygen affinity. Oxyhemoglobin maintains a planar heme structure allowing cooperative oxygen binding and efficient oxygen transport in red blood cells.
Physiological Roles in Oxygen Transport
Methemoglobin contains iron in the ferric (Fe3+) state, preventing it from binding oxygen, which reduces oxygen delivery efficiency to tissues. Oxyhemoglobin, with iron in the ferrous (Fe2+) state, binds oxygen reversibly, facilitating transport from lungs to peripheral tissues. The balance between these forms is crucial for maintaining adequate oxygen transport and preventing hypoxia.
Causes of Methemoglobin Formation
Methemoglobin forms when the ferrous iron (Fe2+) in hemoglobin is oxidized to ferric iron (Fe3+), impairing oxygen binding and transport. Common causes include exposure to oxidizing agents such as nitrates, certain medications like dapsone and benzocaine, and genetic enzyme deficiencies affecting cytochrome b5 reductase. This abnormal form of hemoglobin leads to decreased oxygen delivery to tissues, resulting in methemoglobinemia.
Clinical Implications and Symptoms
Methemoglobin, an oxidized form of hemoglobin, impairs oxygen delivery by reducing the blood's oxygen-carrying capacity, leading to tissue hypoxia and cyanosis. Elevated methemoglobin levels, typically above 1-2%, cause symptoms such as headache, fatigue, dyspnea, and at higher concentrations, neurological deficits and cardiovascular collapse. Oxyhemoglobin represents hemoglobin bound to oxygen, essential for effective oxygen transport, and abnormalities in its levels directly reflect respiratory or circulatory disorders requiring immediate clinical intervention.
Diagnostic Approaches and Detection Methods
Methemoglobin is detected through co-oximetry, a specialized spectrophotometric technique that differentiates it from oxyhemoglobin by analyzing multiple wavelengths of light absorption. Pulse oximetry, commonly used for oxyhemoglobin, cannot accurately quantify methemoglobin due to overlapping absorption spectra, necessitating blood gas analysis with co-oximeters for precise diagnosis. Advanced diagnostic approaches also include spectrophotometric assays and reflectance spectroscopy, which provide rapid and reliable detection of methemoglobinemia levels compared to traditional oxygen saturation measurements.
Treatment of Methemoglobinemia
Treatment of methemoglobinemia primarily involves the administration of methylene blue, a reducing agent that converts methemoglobin back to functional oxyhemoglobin. In severe cases, supplemental oxygen therapy enhances tissue oxygenation despite impaired hemoglobin function. Exchange transfusion or hyperbaric oxygen therapy may be necessary when standard treatments fail or in cases of significant methemoglobin elevation.
Key Differences and Summary Table
Methemoglobin contains iron in the ferric (Fe3+) state, impairing its ability to bind oxygen, whereas oxyhemoglobin contains iron in the ferrous (Fe2+) state, effectively transporting oxygen to tissues. Methemoglobin causes reduced oxygen delivery and cyanosis even when oxygen levels in blood are adequate, while oxyhemoglobin supports normal oxygen transport and tissue oxygenation. A summary table highlights methemoglobin's oxidized iron form, impaired oxygen binding, and clinical relevance in methemoglobinemia versus oxyhemoglobin's reduced iron form, effective oxygen transport, and central role in respiration.
Methemoglobin Infographic
 libterm.com
libterm.com