Antifungal treatments target fungal infections by inhibiting the growth and reproduction of harmful fungi on the skin, nails, or internal organs. These medications come in various forms, including creams, ointments, tablets, and shampoos, designed to effectively eliminate fungal pathogens and relieve symptoms such as itching, redness, and discomfort. Discover how you can protect yourself and choose the right antifungal solution by reading the rest of the article.
Table of Comparison
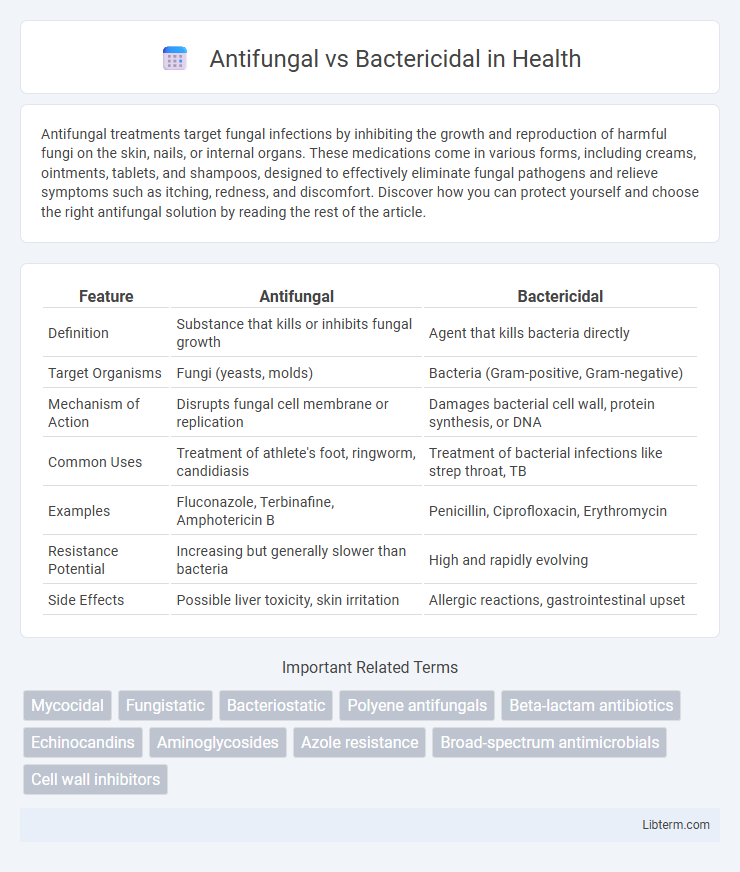
| Feature | Antifungal | Bactericidal |
|---|---|---|
| Definition | Substance that kills or inhibits fungal growth | Agent that kills bacteria directly |
| Target Organisms | Fungi (yeasts, molds) | Bacteria (Gram-positive, Gram-negative) |
| Mechanism of Action | Disrupts fungal cell membrane or replication | Damages bacterial cell wall, protein synthesis, or DNA |
| Common Uses | Treatment of athlete's foot, ringworm, candidiasis | Treatment of bacterial infections like strep throat, TB |
| Examples | Fluconazole, Terbinafine, Amphotericin B | Penicillin, Ciprofloxacin, Erythromycin |
| Resistance Potential | Increasing but generally slower than bacteria | High and rapidly evolving |
| Side Effects | Possible liver toxicity, skin irritation | Allergic reactions, gastrointestinal upset |
Understanding Antifungal and Bactericidal Agents
Antifungal agents target fungal infections by disrupting fungal cell membranes or interfering with essential fungal enzymes, effectively eliminating or inhibiting fungal growth. Bactericidal agents kill bacteria directly through mechanisms such as cell wall synthesis inhibition or DNA replication interference. Understanding these agents involves recognizing their specific targets and modes of action, which guide appropriate clinical use against fungal or bacterial pathogens.
Key Differences in Mechanisms of Action
Antifungal agents target the unique components of fungal cells, such as ergosterol in the cell membrane, disrupting membrane integrity and inhibiting cell growth. Bactericidal drugs kill bacteria by interfering with essential processes like cell wall synthesis, protein production, or DNA replication, leading to bacterial cell death. The key difference lies in antifungals acting on eukaryotic fungal cells, while bactericidals specifically target prokaryotic bacterial structures and functions.
Target Organisms: Fungi vs Bacteria
Antifungal agents specifically target fungi, including yeasts and molds, by disrupting their cell membranes or interfering with essential cellular processes unique to fungal cells. Bactericidal drugs act against bacteria by killing the bacteria outright, often by targeting bacterial cell walls, protein synthesis, or DNA replication. The fundamental distinction lies in their target organisms: antifungals are effective against fungal infections, while bactericidals eliminate bacterial pathogens.
Common Antifungal Medications
Common antifungal medications include fluconazole, itraconazole, and terbinafine, which target fungal cell membranes or cell walls to inhibit growth. These drugs are effective against a variety of fungal infections such as candidiasis, dermatophytosis, and onychomycosis. Unlike bactericidal agents that kill bacteria directly, antifungals primarily disrupt fungal metabolism or reproduction.
Popular Bactericidal Antibiotics
Popular bactericidal antibiotics include penicillins, cephalosporins, fluoroquinolones, and aminoglycosides, all of which actively kill bacteria by targeting cell wall synthesis, DNA replication, or protein synthesis. In contrast, antifungal agents such as azoles and echinocandins inhibit fungal cell membrane or cell wall synthesis without directly killing fungi but rather inhibiting their growth. Understanding the distinction between bactericidal antibiotics and antifungal drugs is crucial for effective treatment of bacterial versus fungal infections.
Indications and Clinical Applications
Antifungal agents target fungal infections such as candidiasis, aspergillosis, and dermatophytosis, commonly prescribed in conditions like oral thrush, systemic mycoses, and onychomycosis. Bactericidal drugs are effective against bacterial infections including pneumonia, urinary tract infections, and sepsis by actively killing bacteria, with widespread use in treating Staphylococcus aureus and Streptococcus pneumoniae infections. Clinical applications depend on pathogen type, with antifungals used for fungal cell membrane disruption while bactericidal agents interfere with bacterial cell wall synthesis or protein production.
Side Effects and Safety Considerations
Antifungal medications often cause side effects such as liver toxicity, gastrointestinal upset, and skin rashes, requiring monitoring of liver function during prolonged use, while bactericidal drugs commonly lead to gastrointestinal disturbances, allergic reactions, and in some cases, nephrotoxicity or ototoxicity, especially with aminoglycosides. Safety considerations for antifungals include assessing liver health and potential drug interactions due to cytochrome P450 enzyme involvement, whereas bactericidal agents demand caution in patients with renal impairment and careful dosing to prevent resistance and toxicity. Both classes necessitate thorough evaluation of patient history and concurrent medications to minimize adverse effects and ensure therapeutic efficacy.
Resistance: Antifungal vs Bacterial Resistance
Antifungal resistance emerges from genetic mutations and adaptive mechanisms in fungi, often leading to multidrug-resistant strains like Candida auris. In contrast, bacterial resistance develops rapidly through horizontal gene transfer and selective pressure, resulting in widespread multidrug-resistant bacteria such as MRSA and carbapenem-resistant Enterobacteriaceae. Understanding these distinct resistance pathways is crucial for developing targeted therapies and stewardship strategies to combat infections effectively.
Choosing the Right Treatment: Factors to Consider
Choosing the right treatment between antifungal and bactericidal agents depends on accurately identifying the infection type, as antifungal medications target fungal infections while bactericidal drugs eliminate bacterial pathogens. Consider factors such as the infection's location, severity, patient immune status, and potential drug resistance when selecting therapy. Laboratory tests like cultures and sensitivity assays help guide effective treatment decisions to ensure optimal outcomes and minimize adverse effects.
Future Trends in Antifungal and Bactericidal Therapy
Future trends in antifungal and bactericidal therapy emphasize the development of novel agents targeting drug-resistant strains and biofilms, utilizing advanced molecular techniques such as CRISPR and nanotechnology for precise delivery and enhanced efficacy. Innovations in combination therapies are gaining traction, integrating antifungal and bactericidal compounds to combat polymicrobial infections effectively and reduce the emergence of resistance. Personalized medicine approaches, leveraging genomics and microbiome analysis, are set to optimize treatment regimens, improving patient outcomes in fungal and bacterial infections.
Antifungal Infographic
 libterm.com
libterm.com