Ketoacidosis is a serious metabolic condition characterized by high levels of ketones in the blood, resulting from uncontrolled diabetes or prolonged fasting. This imbalance causes the blood to become acidic, leading to symptoms such as nausea, vomiting, abdominal pain, and confusion. Discover critical insights into ketoacidosis, its causes, symptoms, and effective treatment options by reading the rest of the article.
Table of Comparison
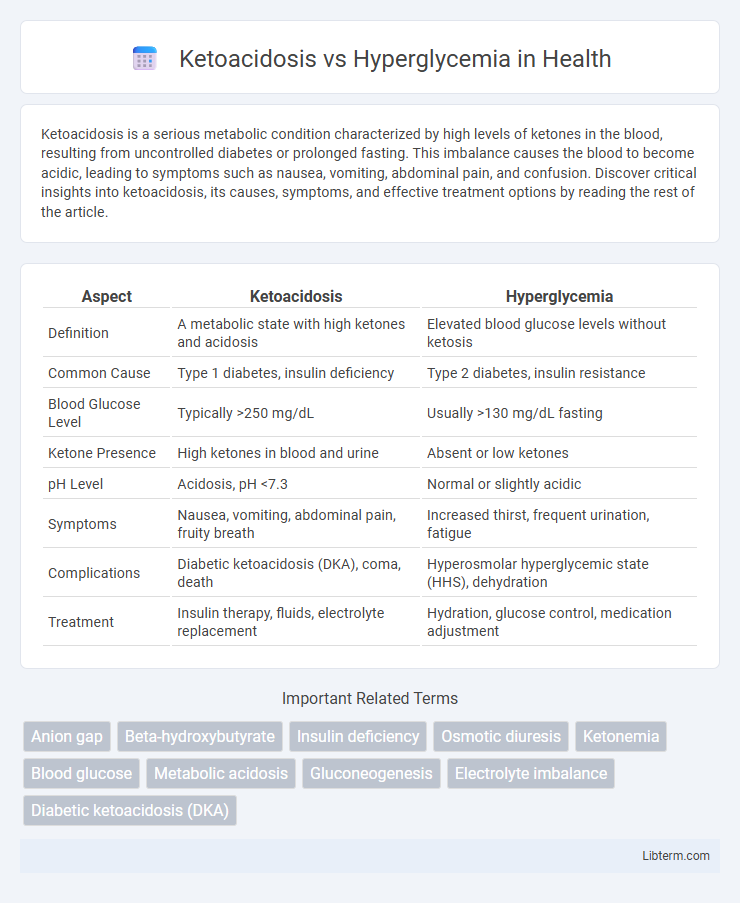
| Aspect | Ketoacidosis | Hyperglycemia |
|---|---|---|
| Definition | A metabolic state with high ketones and acidosis | Elevated blood glucose levels without ketosis |
| Common Cause | Type 1 diabetes, insulin deficiency | Type 2 diabetes, insulin resistance |
| Blood Glucose Level | Typically >250 mg/dL | Usually >130 mg/dL fasting |
| Ketone Presence | High ketones in blood and urine | Absent or low ketones |
| pH Level | Acidosis, pH <7.3 | Normal or slightly acidic |
| Symptoms | Nausea, vomiting, abdominal pain, fruity breath | Increased thirst, frequent urination, fatigue |
| Complications | Diabetic ketoacidosis (DKA), coma, death | Hyperosmolar hyperglycemic state (HHS), dehydration |
| Treatment | Insulin therapy, fluids, electrolyte replacement | Hydration, glucose control, medication adjustment |
Introduction to Ketoacidosis and Hyperglycemia
Ketoacidosis is a dangerous metabolic condition characterized by elevated ketone bodies and acidosis, commonly associated with uncontrolled diabetes mellitus type 1. Hyperglycemia refers to abnormally high blood glucose levels exceeding 130 mg/dL fasting or 180 mg/dL postprandial, often indicating insufficient insulin activity or resistance. Both conditions require prompt medical intervention to prevent severe complications such as diabetic ketoacidosis (DKA) or hyperosmolar hyperglycemic state (HHS).
Definition and Key Differences
Ketoacidosis is a severe metabolic condition characterized by high blood ketone levels and acidosis, commonly seen in uncontrolled type 1 diabetes, whereas hyperglycemia refers to elevated blood glucose levels without necessarily causing acidosis. Ketoacidosis involves ketone body accumulation and significant electrolyte imbalances, leading to symptoms like nausea, vomiting, and rapid breathing, while hyperglycemia primarily manifests as increased thirst, frequent urination, and fatigue. Key differences include the presence of ketones and acidosis in ketoacidosis, which require immediate medical intervention, contrasting with hyperglycemia that often results from insufficient insulin or insulin resistance.
Causes and Risk Factors
Ketoacidosis primarily occurs due to insulin deficiency, commonly seen in type 1 diabetes, leading to excessive fat breakdown and ketone buildup. Hyperglycemia results from insufficient insulin or insulin resistance, frequently associated with type 2 diabetes and poor dietary choices. Risk factors for ketoacidosis include infection, missed insulin doses, and stress, while hyperglycemia risk factors encompass obesity, sedentary lifestyle, and chronic illnesses.
Clinical Symptoms Comparison
Ketoacidosis typically presents with symptoms such as nausea, vomiting, abdominal pain, rapid breathing, and a distinct fruity odor on the breath, reflecting the body's attempt to expel excess ketones. Hyperglycemia symptoms include increased thirst, frequent urination, blurred vision, and fatigue, primarily due to elevated blood glucose levels without significant ketone accumulation. Distinguishing between these clinical manifestations is crucial for timely diagnosis and appropriate management of diabetic emergencies.
Diagnostic Criteria and Laboratory Findings
Ketoacidosis is characterized by blood glucose levels above 250 mg/dL, arterial pH less than 7.3, serum bicarbonate below 18 mEq/L, and positive serum or urine ketones, indicating metabolic acidosis due to ketone accumulation. Hyperglycemia presents with elevated blood glucose exceeding 180 mg/dL without significant ketone production or acidosis, and typically normal arterial pH and bicarbonate levels. Laboratory findings in ketoacidosis include high anion gap metabolic acidosis, elevated serum ketones, and hyperglycemia, while hyperglycemia primarily shows elevated glucose with normal acid-base status and absent or minimal ketones.
Acute Complications
Ketoacidosis, primarily seen in type 1 diabetes, involves severe insulin deficiency causing elevated ketone levels, metabolic acidosis, and dehydration, often resulting in rapid onset acute complications like diabetic ketoacidosis (DKA). Hyperglycemia, characterized by high blood glucose levels, can lead to hyperosmolar hyperglycemic state (HHS) in type 2 diabetes, marked by extreme hyperglycemia, severe dehydration, and neurological impairments. Both conditions require urgent medical intervention to prevent life-threatening sequelae such as coma, electrolyte imbalances, and organ failure.
Treatment Approaches
Treatment of ketoacidosis primarily involves intravenous insulin administration to reduce blood glucose and halt ketone production, alongside fluid replacement to correct dehydration and electrolyte imbalances, particularly potassium. Hyperglycemia management focuses on oral hypoglycemic agents or subcutaneous insulin, emphasizing lifestyle modifications such as diet and exercise to maintain blood sugar within target ranges. Monitoring and adjusting treatment based on blood glucose levels and underlying causes is essential for both conditions to prevent complications and ensure effective glucose control.
Prevention Strategies
Prevention strategies for ketoacidosis emphasize strict blood glucose monitoring, timely insulin administration, and avoiding prolonged fasting to maintain metabolic balance and prevent ketone buildup. For hyperglycemia, consistent carbohydrate counting, regular exercise, and adherence to prescribed medication regimens are essential to stabilize blood sugar levels and minimize spikes. Patient education on recognizing early symptoms and maintaining routine healthcare visits significantly reduces the risk of severe complications in both conditions.
Prognosis and Long-term Outcomes
Ketoacidosis, particularly diabetic ketoacidosis (DKA), presents an acute medical emergency with a higher immediate mortality risk but can lead to full recovery if promptly treated. Hyperglycemia, often chronic, contributes to long-term complications such as cardiovascular disease, neuropathy, and nephropathy, significantly affecting prognosis over time. Effective glucose management and early intervention are crucial for improving long-term outcomes in both conditions, reducing the risk of recurrent episodes and chronic complications.
When to Seek Medical Help
Seek immediate medical help for ketoacidosis when symptoms such as rapid breathing, fruity-smelling breath, confusion, or persistent vomiting occur, as it indicates dangerously high ketone levels and requires urgent treatment. Hyperglycemia demands prompt medical attention if blood glucose remains consistently above 240 mg/dL, especially with signs of frequent urination, increased thirst, or fatigue, to prevent progression to diabetic emergencies. Recognizing these critical symptoms early supports timely intervention, reducing the risk of severe complications like diabetic ketoacidosis or hyperosmolar hyperglycemic state.
Ketoacidosis Infographic
 libterm.com
libterm.com