Immunosuppression reduces the effectiveness of your immune system, increasing vulnerability to infections and diseases. It can be caused by medical treatments, such as chemotherapy or organ transplants, or by certain health conditions. Discover how immunosuppression impacts your health and learn strategies to manage its effects in the rest of this article.
Table of Comparison
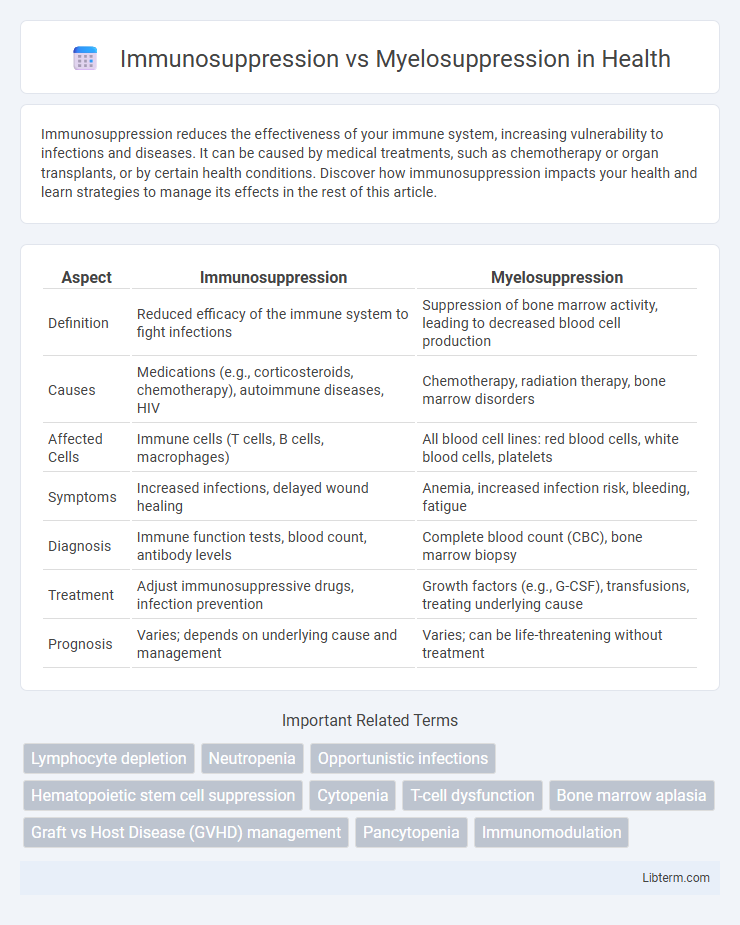
| Aspect | Immunosuppression | Myelosuppression |
|---|---|---|
| Definition | Reduced efficacy of the immune system to fight infections | Suppression of bone marrow activity, leading to decreased blood cell production |
| Causes | Medications (e.g., corticosteroids, chemotherapy), autoimmune diseases, HIV | Chemotherapy, radiation therapy, bone marrow disorders |
| Affected Cells | Immune cells (T cells, B cells, macrophages) | All blood cell lines: red blood cells, white blood cells, platelets |
| Symptoms | Increased infections, delayed wound healing | Anemia, increased infection risk, bleeding, fatigue |
| Diagnosis | Immune function tests, blood count, antibody levels | Complete blood count (CBC), bone marrow biopsy |
| Treatment | Adjust immunosuppressive drugs, infection prevention | Growth factors (e.g., G-CSF), transfusions, treating underlying cause |
| Prognosis | Varies; depends on underlying cause and management | Varies; can be life-threatening without treatment |
Introduction to Immunosuppression and Myelosuppression
Immunosuppression refers to the reduction or inhibition of the immune system's ability to fight infections and diseases, often induced intentionally through medications like corticosteroids or chemotherapy to prevent organ transplant rejection or treat autoimmune diseases. Myelosuppression specifically targets the bone marrow's capacity to produce blood cells, leading to decreased levels of red blood cells, white blood cells, and platelets, which can result in anemia, increased infection risk, and bleeding disorders. Both conditions are critical considerations in clinical settings due to their impact on patient immunity and hematologic health.
Defining Immunosuppression: Mechanisms and Causes
Immunosuppression refers to the reduction or inhibition of the immune system's ability to fight infections and diseases, often caused by medications such as corticosteroids, chemotherapy agents, or conditions like HIV/AIDS. It involves the suppression of immune cell function, including T cells, B cells, and macrophages, leading to increased susceptibility to infections and malignancies. Unlike myelosuppression, which specifically affects bone marrow cell production, immunosuppression targets the functional response of immune cells throughout the body.
Understanding Myelosuppression: Key Processes
Myelosuppression is a critical condition characterized by the decreased production of blood cells due to bone marrow suppression, impacting red cells, white cells, and platelets. This reduction in hematopoietic activity leads to anemia, increased infection risk, and bleeding tendencies, distinguishing it from immunosuppression, which primarily affects immune system functionality without directly reducing blood cell counts. Understanding the mechanisms of myelosuppression involves recognizing the bone marrow's vulnerability to chemotherapy, radiation, and certain medications that disrupt normal cell proliferation and differentiation.
Major Differences Between Immunosuppression and Myelosuppression
Immunosuppression primarily involves the reduction or inhibition of immune system activity, often through medications or diseases targeting immune cells, leading to increased vulnerability to infections. Myelosuppression refers to the decreased production of bone marrow cells, including red blood cells, white blood cells, and platelets, resulting in anemia, leukopenia, and thrombocytopenia. The major difference lies in immunosuppression affecting immune function specifically, while myelosuppression broadly impacts hematopoiesis and all blood cell lineages.
Common Causes and Risk Factors
Immunosuppression commonly results from factors such as HIV infection, chemotherapy, corticosteroid use, and organ transplantation, which impair the immune system's ability to fight infections. Myelosuppression typically arises due to chemotherapy, radiation therapy, certain medications, and bone marrow disorders, leading to decreased production of blood cells. Risk factors for both conditions include advanced age, underlying chronic illnesses, and concurrent use of immunosuppressive agents or cytotoxic drugs.
Clinical Manifestations and Symptoms
Immunosuppression results in increased susceptibility to infections, characterized by frequent fevers, opportunistic infections, and delayed wound healing due to compromised immune cell function. Myelosuppression primarily manifests as anemia, leukopenia, and thrombocytopenia, leading to symptoms such as fatigue, pallor, easy bruising, bleeding tendencies, and increased infection risk from reduced white blood cell counts. Clinical evaluation reveals overlapping signs of immunodeficiency, but specific blood count abnormalities differentiate myelosuppression from generalized immunosuppression.
Diagnostic Approaches: Identifying Each Condition
Immunosuppression is diagnosed through immune function tests such as lymphocyte subset analysis, immunoglobulin levels, and assessment of cytokine production, while myelosuppression is identified via complete blood counts (CBC) showing decreased levels of red cells, white cells, and platelets. Bone marrow biopsy and aspiration serve as definitive diagnostic tools to evaluate marrow cellularity and identify causes of hematopoietic suppression. Flow cytometry and molecular genetic testing further differentiate underlying etiologies, guiding targeted treatment strategies.
Impact on Patient Health and Outcomes
Immunosuppression reduces the immune system's ability to fight infections, increasing patient susceptibility to opportunistic pathogens and prolonging recovery times. Myelosuppression specifically impairs bone marrow function, leading to decreased production of blood cells like leukocytes, erythrocytes, and platelets, which can cause anemia, infection risk, and bleeding complications. Both conditions significantly impact patient outcomes by increasing morbidity and necessitating close monitoring and supportive treatments such as growth factors, transfusions, or prophylactic antimicrobials.
Treatment Strategies and Management
Immunosuppression management involves targeted use of corticosteroids, biologics, and immunomodulators to reduce immune system activity while minimizing infection risk, often requiring prophylactic antimicrobials and regular immune function monitoring. Myelosuppression treatment focuses on supportive care including blood transfusions, growth factors like G-CSF or erythropoietin to stimulate bone marrow recovery, and dose adjustments of cytotoxic therapies to prevent prolonged marrow suppression. Close hematological monitoring and individualized therapy adjustments are essential to optimize outcomes and reduce complications in both conditions.
Prevention and Monitoring: Best Practices
Effective prevention of immunosuppression and myelosuppression involves regular blood count monitoring, including complete blood count (CBC) with differential to detect early neutropenia or anemia. Prophylactic measures such as administering growth factors like G-CSF for neutropenia and patient education on infection control significantly reduce complications. Timely dose adjustments of immunosuppressive or myelosuppressive agents and vigilant clinical assessment ensure optimal therapy management and minimize adverse effects.
Immunosuppression Infographic
 libterm.com
libterm.com