Hepatic steatosis, commonly known as fatty liver disease, involves the accumulation of excess fat in liver cells, potentially leading to inflammation and liver damage. Risk factors include obesity, insulin resistance, and excessive alcohol consumption, which can progress to more severe liver conditions if untreated. Learn more about the causes, symptoms, and effective management strategies in the rest of the article.
Table of Comparison
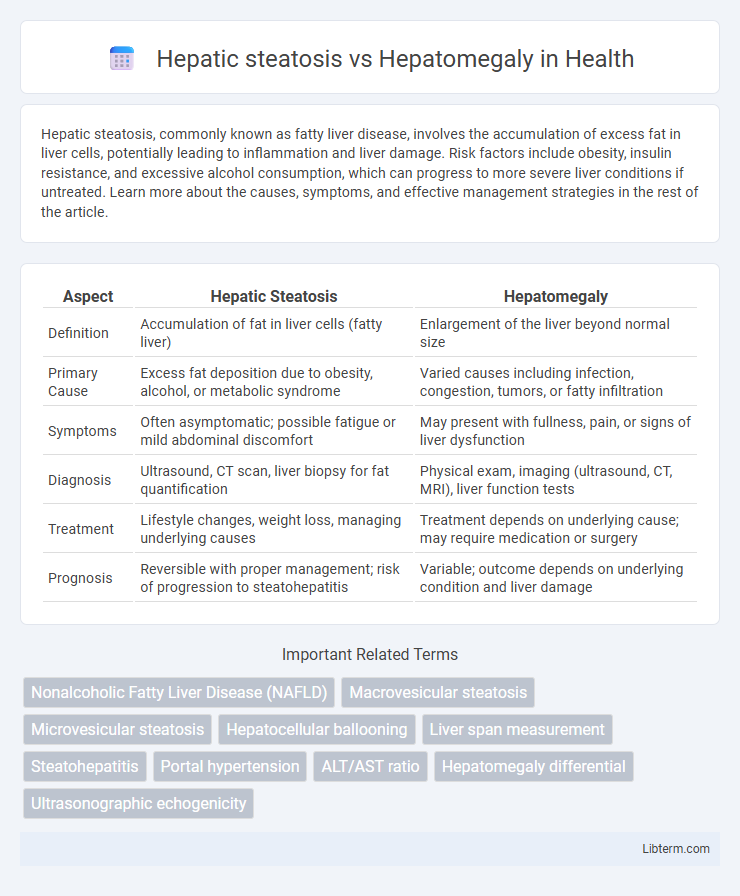
| Aspect | Hepatic Steatosis | Hepatomegaly |
|---|---|---|
| Definition | Accumulation of fat in liver cells (fatty liver) | Enlargement of the liver beyond normal size |
| Primary Cause | Excess fat deposition due to obesity, alcohol, or metabolic syndrome | Varied causes including infection, congestion, tumors, or fatty infiltration |
| Symptoms | Often asymptomatic; possible fatigue or mild abdominal discomfort | May present with fullness, pain, or signs of liver dysfunction |
| Diagnosis | Ultrasound, CT scan, liver biopsy for fat quantification | Physical exam, imaging (ultrasound, CT, MRI), liver function tests |
| Treatment | Lifestyle changes, weight loss, managing underlying causes | Treatment depends on underlying cause; may require medication or surgery |
| Prognosis | Reversible with proper management; risk of progression to steatohepatitis | Variable; outcome depends on underlying condition and liver damage |
Introduction: Understanding Hepatic Steatosis vs Hepatomegaly
Hepatic steatosis is characterized by the accumulation of excess fat in liver cells, leading to fatty liver disease commonly linked to obesity, diabetes, and alcohol consumption. Hepatomegaly refers to the abnormal enlargement of the liver, which can result from various underlying conditions including infections, liver diseases, or congestive heart failure. Differentiating between hepatic steatosis and hepatomegaly is crucial for accurate diagnosis and targeted treatment strategies.
Definition of Hepatic Steatosis
Hepatic steatosis, commonly known as fatty liver disease, is characterized by the excessive accumulation of fat within liver cells, often associated with alcohol use or metabolic conditions such as obesity and diabetes. Hepatomegaly refers to an enlarged liver, which can result from various causes including hepatic steatosis, infections, or congestive heart failure. Understanding hepatic steatosis is crucial, as it represents a key pathological process that can lead to liver inflammation, fibrosis, and potentially cirrhosis if left untreated.
Definition of Hepatomegaly
Hepatomegaly refers to the abnormal enlargement of the liver, which can result from various causes such as infections, liver diseases, or congestive heart failure. Unlike hepatic steatosis, which is characterized by fat accumulation within liver cells, hepatomegaly represents a physical increase in liver size often detected through clinical examination or imaging techniques. Accurate diagnosis of hepatomegaly typically involves ultrasound, CT scan, or MRI to assess liver dimensions and identify underlying pathology.
Pathophysiological Differences
Hepatic steatosis is characterized by excessive accumulation of triglycerides within hepatocytes due to imbalances in lipid metabolism, often linked to insulin resistance and oxidative stress. Hepatomegaly refers to an enlarged liver that can result from various causes including inflammation, congestion, or infiltration, with pathophysiology involving cellular hypertrophy, hyperplasia, or extracellular matrix deposition. While hepatic steatosis primarily affects lipid storage at the cellular level, hepatomegaly reflects a broader spectrum of structural and functional alterations in liver tissue.
Causes and Risk Factors
Hepatic steatosis, commonly known as fatty liver disease, is primarily caused by excessive alcohol consumption, obesity, insulin resistance, and metabolic syndrome, leading to fat accumulation in liver cells. Hepatomegaly refers to an enlarged liver resulting from various conditions such as liver infections, congestive heart failure, or infiltrative diseases like amyloidosis and lymphoma. Risk factors for hepatic steatosis include type 2 diabetes and dyslipidemia, while hepatomegaly risk factors vary depending on the underlying cause but often involve chronic systemic illnesses and liver pathology.
Clinical Manifestations
Hepatic steatosis primarily presents with asymptomatic liver enlargement and mild right upper quadrant discomfort, often detected through imaging or abnormal liver function tests. Hepatomegaly manifests as a palpable, enlarged liver that may cause abdominal fullness, pain, or tenderness, and its clinical features vary depending on the underlying disease. Both conditions can involve elevated liver enzymes, but hepatomegaly is typically associated with systemic symptoms when linked to infections, malignancies, or congestive heart failure.
Diagnostic Approaches
Hepatic steatosis is diagnosed primarily through imaging techniques such as ultrasound, CT scan, or MRI that reveal fat accumulation in liver cells, while liver biopsy remains the gold standard for confirming the extent of fat infiltration. Hepatomegaly, characterized by an enlarged liver, is typically identified using physical examination and confirmed by imaging modalities like ultrasound or CT to assess liver size and detect underlying causes such as inflammation or tumors. Blood tests including liver function tests and biomarkers support the differentiation of hepatic steatosis from hepatomegaly by indicating liver damage or metabolic disturbances.
Imaging and Laboratory Findings
Hepatic steatosis typically appears as increased echogenicity on ultrasound and shows low attenuation on CT scans, with MRI demonstrating signal drop using fat-saturation techniques; laboratory findings often reveal mildly elevated ALT and AST levels. Hepatomegaly, detectable through ultrasound, CT, or MRI as enlargement of the liver without specific fat infiltration patterns, can be associated with various pathologies and may present with normal or elevated liver enzymes depending on the underlying cause. Differentiating these conditions involves correlating imaging features--fat content in steatosis versus size increase in hepatomegaly--and evaluating liver function tests for inflammation or damage markers.
Treatment and Management Strategies
Treatment of hepatic steatosis primarily involves lifestyle modifications such as weight loss, dietary changes, and increased physical activity to reduce liver fat accumulation and improve insulin sensitivity. Management of hepatomegaly depends on the underlying cause, including treating infections, controlling congestive heart failure, or addressing liver diseases like hepatitis or cirrhosis with appropriate medications and interventions. Regular monitoring through imaging and liver function tests is essential in both conditions to assess treatment efficacy and prevent progression to advanced liver damage.
Prognosis and Potential Complications
Hepatic steatosis primarily presents with fat accumulation in liver cells, often reversible with lifestyle changes, but can progress to nonalcoholic steatohepatitis (NASH) and cirrhosis, increasing risk of liver failure and hepatocellular carcinoma. Hepatomegaly indicates an enlarged liver caused by various conditions including infection, congestion, or malignancy, with prognosis dependent on underlying etiology and potential complications like liver dysfunction or portal hypertension. Timely diagnosis and management are critical to prevent irreversible liver damage and associated systemic complications in both conditions.
Hepatic steatosis Infographic
 libterm.com
libterm.com