Understanding bioequivalence and bioavailability is crucial for evaluating how drugs perform in the body, ensuring that generic medications match the effectiveness of their branded counterparts. Bioavailability measures the rate and extent of active drug absorption, while bioequivalence ensures that two products release the drug into the bloodstream at similar rates and amounts. Explore the rest of this article to deepen your knowledge about how these concepts impact drug development and therapeutic effectiveness.
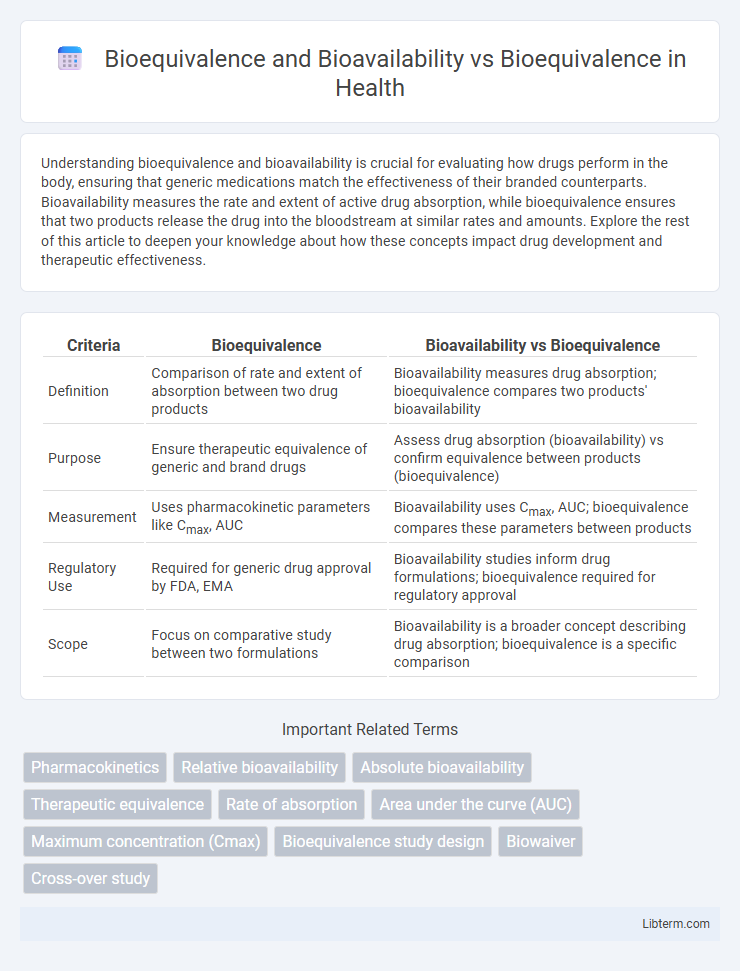
Table of Comparison
| Criteria | Bioequivalence | Bioavailability vs Bioequivalence |
|---|---|---|
| Definition | Comparison of rate and extent of absorption between two drug products | Bioavailability measures drug absorption; bioequivalence compares two products' bioavailability |
| Purpose | Ensure therapeutic equivalence of generic and brand drugs | Assess drug absorption (bioavailability) vs confirm equivalence between products (bioequivalence) |
| Measurement | Uses pharmacokinetic parameters like Cmax, AUC | Bioavailability uses Cmax, AUC; bioequivalence compares these parameters between products |
| Regulatory Use | Required for generic drug approval by FDA, EMA | Bioavailability studies inform drug formulations; bioequivalence required for regulatory approval |
| Scope | Focus on comparative study between two formulations | Bioavailability is a broader concept describing drug absorption; bioequivalence is a specific comparison |
Understanding Bioavailability: Definition and Significance
Bioavailability refers to the proportion of a drug that enters systemic circulation and reaches the target site, ensuring optimal therapeutic effect. Understanding bioavailability is crucial in drug development and clinical pharmacology because it influences dosing, efficacy, and safety profiles. Distinguishing bioavailability from bioequivalence is essential, as bioequivalence compares the bioavailability between different formulations to guarantee therapeutic consistency.
What is Bioequivalence? Core Principles Explained
Bioequivalence refers to the absence of a significant difference in the rate and extent to which the active ingredient of a drug becomes available at the site of action when administered under similar conditions. It ensures that two pharmaceutical products, typically a generic and its branded counterpart, deliver the same amount of active ingredient into a patient's bloodstream in the same time frame, maintaining therapeutic equivalence. Core principles of bioequivalence testing include pharmacokinetic parameter comparison such as Cmax (maximum concentration), Tmax (time to reach Cmax), and AUC (area under the curve), which collectively confirm that the generic product matches the original reference drug in performance.
The Relationship Between Bioavailability and Bioequivalence
Bioavailability measures the extent and rate at which the active drug ingredient is absorbed and becomes available at the site of action, while bioequivalence compares the bioavailability of two pharmaceutical products to ensure therapeutic equivalence. The relationship between bioavailability and bioequivalence is critical for regulatory approval, as bioequivalence studies rely on pharmacokinetic parameters like Cmax and AUC to demonstrate similar bioavailability profiles between a generic and a reference drug. This ensures that the generic product delivers the same efficacy and safety as the original, supporting substitution without compromising clinical outcomes.
Key Differences: Bioavailability vs Bioequivalence
Bioavailability measures the rate and extent to which an active drug ingredient becomes available at the site of action, whereas bioequivalence compares the bioavailability of two pharmaceutical products to ensure therapeutic equivalence. Key differences include bioavailability focusing on a single drug's absorption and systemic availability, while bioequivalence assesses if two formulations release the active ingredient into the bloodstream at similar rates and extents. Regulatory agencies require bioequivalence studies to approve generic drugs by demonstrating no significant difference in bioavailability from the branded counterpart.
Regulatory Guidelines for Bioequivalence Studies
Regulatory guidelines for bioequivalence studies emphasize the rigorous assessment of both bioavailability and bioequivalence to ensure therapeutic equivalence between generic and reference drug products. Agencies like the FDA and EMA require specific pharmacokinetic parameters such as Cmax and AUC within defined confidence intervals, typically 80-125%, to demonstrate bioequivalence. These guidelines mandate standardized study designs, including crossover trials in healthy volunteers, to minimize variability and reliably compare the rate and extent of absorption.
Criteria for Assessing Bioavailability
Criteria for assessing bioavailability primarily include the rate and extent of drug absorption, measured through parameters such as Cmax (maximum concentration), Tmax (time to reach Cmax), and AUC (area under the concentration-time curve). Bioavailability quantifies the fraction of an administered dose reaching systemic circulation, whereas bioequivalence compares the bioavailability between two pharmaceutical products to ensure therapeutic equivalence. Bioequivalence studies rely on statistical analysis of pharmacokinetic parameters to confirm that generic and brand-name drugs fall within an acceptable range, usually 80-125% for AUC and Cmax.
Methods Used in Bioequivalence Testing
Bioequivalence testing primarily employs pharmacokinetic methods such as measuring the rate and extent of drug absorption through parameters like Cmax, Tmax, and AUC obtained from plasma concentration-time curves. Techniques including crossover study designs with healthy volunteers, high-performance liquid chromatography (HPLC), and liquid chromatography-mass spectrometry (LC-MS) are standard for accurate quantification of drug levels. Advanced statistical analyses ensure that test and reference products meet regulatory bioequivalence criteria by comparing these pharmacokinetic metrics within defined confidence intervals.
Bioequivalence vs Therapeutic Equivalence
Bioequivalence compares the rate and extent of drug absorption between a generic product and its brand-name counterpart to ensure similar bioavailability. Therapeutic equivalence extends beyond bioequivalence by confirming that the generic drug not only matches pharmacokinetic parameters but also produces the same clinical effect and safety profile. Regulatory agencies require both bioequivalence and therapeutic equivalence to approve generic medications as interchangeable with brand-name drugs.
Challenges in Evaluating Bioavailability and Bioequivalence
Evaluating bioavailability presents challenges such as variability in drug absorption due to physiological differences and formulation complexities, which can obscure true drug exposure measurements. Bioequivalence studies must control for these variables to ensure that two drug products deliver the same active ingredient at equivalent rates and extents. Accurate assessment relies on sensitive analytical methods and robust pharmacokinetic modeling to address inter-individual variability and simulate real-world drug performance.
Importance of Bioavailability and Bioequivalence in Generic Drug Approval
Bioavailability measures the rate and extent to which the active drug ingredient is absorbed and becomes available at the site of action, while bioequivalence ensures that two drug products have comparable bioavailability and therapeutic effects. The importance of bioavailability and bioequivalence in generic drug approval lies in guaranteeing that generic medications provide the same efficacy and safety as their branded counterparts. Regulatory agencies rely on these parameters to confirm that generics meet quality standards, thus ensuring interchangeability and confidence in generic therapies.
Bioequivalence and Bioavailability Infographic
 libterm.com
libterm.com