Infectious diseases spread rapidly through contact with pathogens such as viruses, bacteria, or fungi, posing significant health risks worldwide. Effective prevention and treatment strategies are crucial to control outbreaks and protect communities. Explore this article to understand how infectious diseases impact your well-being and the measures you can take to stay safe.
Table of Comparison
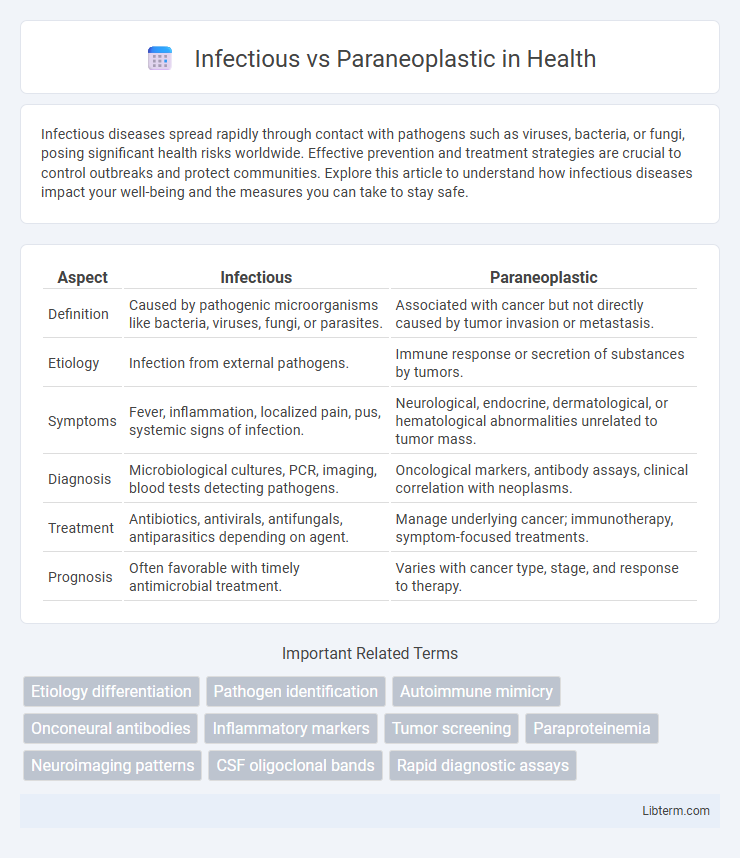
| Aspect | Infectious | Paraneoplastic |
|---|---|---|
| Definition | Caused by pathogenic microorganisms like bacteria, viruses, fungi, or parasites. | Associated with cancer but not directly caused by tumor invasion or metastasis. |
| Etiology | Infection from external pathogens. | Immune response or secretion of substances by tumors. |
| Symptoms | Fever, inflammation, localized pain, pus, systemic signs of infection. | Neurological, endocrine, dermatological, or hematological abnormalities unrelated to tumor mass. |
| Diagnosis | Microbiological cultures, PCR, imaging, blood tests detecting pathogens. | Oncological markers, antibody assays, clinical correlation with neoplasms. |
| Treatment | Antibiotics, antivirals, antifungals, antiparasitics depending on agent. | Manage underlying cancer; immunotherapy, symptom-focused treatments. |
| Prognosis | Often favorable with timely antimicrobial treatment. | Varies with cancer type, stage, and response to therapy. |
Understanding Infectious and Paraneoplastic Diseases
Understanding infectious diseases involves recognizing their causation by pathogens such as bacteria, viruses, fungi, or parasites, which lead to acute or chronic symptoms based on the body's immune response. Paraneoplastic syndromes arise from indirect effects of malignancies, where immune-mediated or hormonal factors cause systemic manifestations unlinked to direct tumor invasion. Accurate diagnosis requires differentiating pathogen-specific markers from tumor-related antibodies, guiding targeted treatment strategies for both infectious and paraneoplastic conditions.
Key Differences Between Infectious and Paraneoplastic Syndromes
Infectious syndromes result from direct microbial invasion and replication leading to symptoms like fever, inflammation, and localized tissue damage, whereas paraneoplastic syndromes are immune-mediated or hormonal responses triggered by an underlying malignancy without direct tumor invasion. Infectious conditions often involve pathogens such as bacteria, viruses, or fungi, while paraneoplastic syndromes are associated with cancer types like lung, breast, or hematologic malignancies. Diagnostic differentiation relies on identifying infectious agents through cultures or PCR and detecting tumor markers or antibodies related to paraneoplastic phenomena.
Common Causes of Infectious Diseases
Common causes of infectious diseases include bacteria such as Streptococcus and Staphylococcus species, viruses like influenza and HIV, fungi including Candida, and parasites such as Plasmodium species responsible for malaria. These pathogens invade the body, leading to symptoms that can mimic paraneoplastic syndromes but are directly linked to infectious agents. Accurate identification of infectious causes through laboratory testing is essential for effective treatment and distinguishing them from paraneoplastic conditions.
Triggers and Mechanisms of Paraneoplastic Syndromes
Paraneoplastic syndromes are triggered by an immune response to tumor antigens expressed by cancer cells, leading to the production of autoantibodies or T-cell activation against both tumor and normal tissues. These mechanisms differ from infectious syndromes, which result from direct microbial invasion and toxin production causing tissue damage. Understanding the role of onconeural antigens and molecular mimicry in paraneoplastic syndromes is critical for distinguishing them from infectious causes and guiding appropriate treatment strategies.
Diagnostic Approaches: Infectious vs Paraneoplastic
Diagnostic approaches for infectious conditions prioritize pathogen identification through cultures, PCR, and serological tests targeting specific microbial agents responsible for symptoms. Paraneoplastic diagnostics emphasize detecting underlying malignancies by leveraging imaging studies like CT or PET scans, alongside tumor marker analysis and biopsy to confirm neoplastic activity. Immunological assays help differentiate autoimmune responses linked to paraneoplastic syndromes from direct infectious causes, guiding targeted therapeutic strategies.
Clinical Manifestations and Overlapping Symptoms
Infectious and paraneoplastic syndromes both present with diverse clinical manifestations, often including fever, weight loss, and neurological deficits, which complicate differential diagnosis. Infectious diseases frequently exhibit signs of systemic inflammation, such as elevated white blood cell counts and positive cultures, whereas paraneoplastic syndromes are characterized by immune-mediated responses secondary to malignancies, commonly affecting the nervous system, skin, and endocrine organs. Overlapping symptoms like fatigue, muscle weakness, and neuropathies require comprehensive diagnostic assessments including imaging, serological markers, and biopsy to distinguish underlying infectious etiologies from paraneoplastic processes.
Laboratory Findings and Biomarkers
Infectious diseases often present elevated inflammatory markers such as C-reactive protein (CRP) and procalcitonin, alongside positive blood cultures or pathogen-specific PCR tests. Paraneoplastic syndromes typically reveal tumor-related biomarkers, including onconeural antibodies like anti-Hu and anti-Yo, elevated lactate dehydrogenase (LDH), and abnormal hormone levels linked to underlying malignancies. Distinguishing these conditions relies heavily on integrating laboratory findings with clinical context and targeted biomarker assays.
Treatment Strategies: Infection vs Paraneoplastic Management
Treatment strategies for infectious conditions prioritize targeted antimicrobial therapy based on culture results and pathogen sensitivity, often requiring prolonged courses to ensure eradication. Paraneoplastic management revolves around identifying and treating the underlying malignancy, utilizing surgery, chemotherapy, or radiation to reduce tumor burden and alleviate symptoms. Supportive care tailored to specific paraneoplastic syndromes includes immunosuppressants and symptomatic therapies to manage immune-mediated effects and improve patient quality of life.
Prognosis and Long-Term Outcomes
Infectious conditions often have a variable prognosis depending on the pathogen, timely diagnosis, and effectiveness of treatment, with outcomes ranging from full recovery to chronic complications or mortality. Paraneoplastic syndromes generally indicate an underlying malignancy, leading to a prognosis heavily influenced by cancer stage, type, and response to therapy, often resulting in poorer long-term outcomes. Early detection and management of the primary tumor in paraneoplastic cases improve survival rates, whereas infectious disease outcomes depend on pathogen characteristics and host immune response.
Recent Advances and Future Directions
Recent advances in distinguishing infectious from paraneoplastic syndromes rely heavily on molecular diagnostics and biomarker identification, enabling precise differentiation between pathogen-driven inflammation and tumor-induced immune responses. Emerging techniques such as next-generation sequencing and proteomic profiling facilitate early detection and personalized therapeutic strategies, improving patient outcomes. Future directions emphasize integrating artificial intelligence for diagnostic refinement and developing targeted immunotherapies that address the underlying etiology of these complex conditions.
Infectious Infographic
 libterm.com
libterm.com