Lusitropic effects refer to the heart's ability to relax during diastole, which improves ventricular filling and overall cardiac function. Enhanced lusitropy can be crucial for patients with heart failure or diastolic dysfunction, as it promotes efficient blood circulation. Discover how lusitropic mechanisms impact your heart health and treatment options in the rest of this article.
Table of Comparison
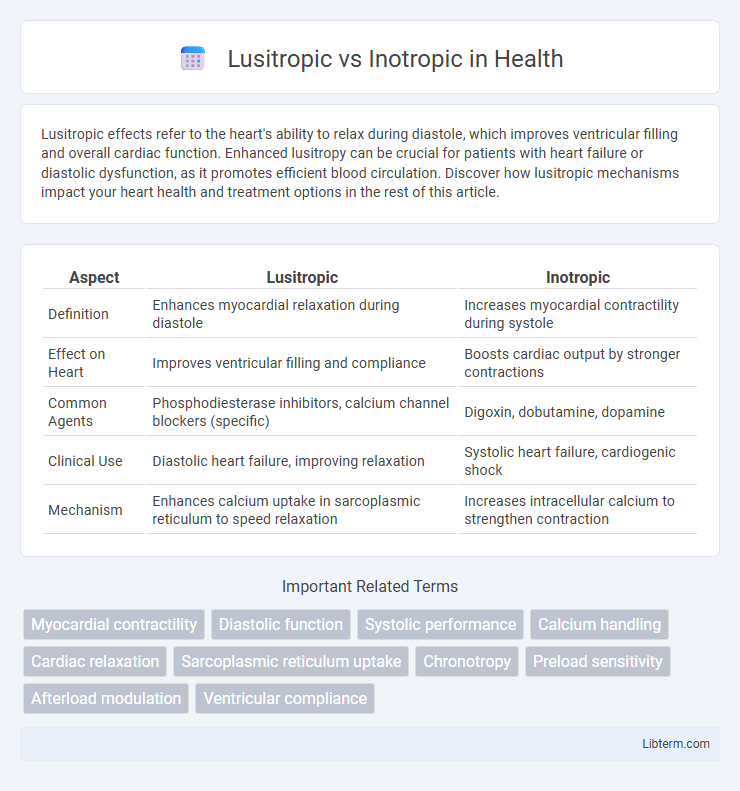
| Aspect | Lusitropic | Inotropic |
|---|---|---|
| Definition | Enhances myocardial relaxation during diastole | Increases myocardial contractility during systole |
| Effect on Heart | Improves ventricular filling and compliance | Boosts cardiac output by stronger contractions |
| Common Agents | Phosphodiesterase inhibitors, calcium channel blockers (specific) | Digoxin, dobutamine, dopamine |
| Clinical Use | Diastolic heart failure, improving relaxation | Systolic heart failure, cardiogenic shock |
| Mechanism | Enhances calcium uptake in sarcoplasmic reticulum to speed relaxation | Increases intracellular calcium to strengthen contraction |
Understanding Lusitropy and Inotropy: Key Definitions
Lusitropy refers to the myocardial relaxation process during diastole, essential for proper ventricular filling and cardiac function, while inotropy denotes the force of myocardial contraction impacting stroke volume and cardiac output. Positive lusitropic effects enhance calcium reuptake by the sarcoplasmic reticulum, facilitating quicker myocardial relaxation, whereas positive inotropic effects increase intracellular calcium availability to strengthen cardiac muscle contraction. Understanding the balance between lusitropic and inotropic mechanisms is critical in managing heart failure and optimizing pharmacological treatment strategies such as beta-adrenergic agonists and calcium channel modulators.
The Physiology Behind Cardiac Contractility
Lusitropic effects refer to the processes that enhance myocardial relaxation during diastole, primarily through improved calcium reuptake by the sarcoplasmic reticulum, allowing for efficient ventricular filling. Inotropic effects involve alterations in the force of myocardial contraction by modulating intracellular calcium availability and sensitivity within cardiac myocytes, directly influencing stroke volume and cardiac output. Understanding the balance between lusitropic and inotropic mechanisms is essential for optimizing cardiac performance and managing conditions like heart failure.
Lusitropic Mechanisms: Enhancing Cardiac Relaxation
Lusitropic mechanisms enhance cardiac relaxation by improving myocardial compliance and accelerating calcium reuptake into the sarcoplasmic reticulum, thereby facilitating efficient ventricular filling during diastole. Key molecular players include the sarcoplasmic reticulum Ca2+-ATPase (SERCA2a) and phospholamban, whose phosphorylation state regulates calcium sequestration speed. Optimizing lusitropy is critical in managing diastolic dysfunction and heart failure with preserved ejection fraction, where impaired relaxation limits cardiac output.
Inotropic Mechanisms: Strengthening Cardiac Contraction
Inotropic mechanisms enhance cardiac contractility by increasing the influx of calcium ions into myocardial cells, which strengthens the force of heart muscle contractions. Positive inotropic agents, such as digitalis and beta-adrenergic agonists, act by boosting intracellular calcium availability, improving stroke volume and cardiac output. This process optimizes heart performance, especially in conditions like heart failure where contractile strength is compromised.
Molecular Pathways: Lusitropy vs Inotropy
Lusitropy enhances myocardial relaxation primarily through phosphorylation of phospholamban by protein kinase A (PKA), which increases sarcoplasmic reticulum calcium ATPase (SERCA) activity, accelerating calcium reuptake into the sarcoplasmic reticulum. Inotropy increases cardiac contractility by elevating intracellular calcium concentration via beta-adrenergic receptor stimulation that activates adenylate cyclase, boosting cAMP levels and PKA activity, which phosphorylates L-type calcium channels and troponin I to enhance calcium availability and myofilament sensitivity. Both pathways converge on PKA-mediated phosphorylation but differ in the downstream targets regulating relaxation (lusitropy) versus contraction (inotropy).
Clinical Significance of Lusitropic and Inotropic Effects
Lusitropic effects refer to the relaxation phase of the cardiac cycle, influencing myocardial relaxation and ventricular filling, which is critical in conditions like diastolic heart failure and hypertrophic cardiomyopathy. Inotropic effects affect myocardial contractility, playing a pivotal role in managing systolic heart failure, shock, and other conditions requiring enhanced cardiac output. Clinically, optimizing lusitropic and inotropic balance helps tailor treatments such as calcium channel blockers for lusitropic improvement and digitalis or beta-agonists for positive inotropic support to improve overall cardiac function.
Pharmacological Agents: Lusitropic and Inotropic Drugs
Lusitropic drugs enhance myocardial relaxation by improving calcium reuptake into the sarcoplasmic reticulum, with agents like beta-blockers and phosphodiesterase inhibitors playing key roles. Inotropic drugs increase myocardial contractility by elevating intracellular calcium levels, exemplified by digoxin, dopamine, and dobutamine. These pharmacological agents are crucial for managing heart failure, with lusitropics targeting diastolic function and inotropics addressing systolic performance.
Heart Failure: The Roles of Lusitropy and Inotropy
Lusitropic and inotropic effects play crucial roles in heart failure management by respectively influencing myocardial relaxation and contractility. Enhanced lusitropy improves ventricular filling and reduces diastolic dysfunction, while increased inotropy strengthens cardiac output by augmenting contractile force. Therapeutic strategies targeting both lusitropic and inotropic pathways optimize cardiac performance and alleviate symptoms in heart failure patients.
Diagnostic Assessment of Lusitropic and Inotropic Function
Diagnostic assessment of lusitropic function evaluates myocardial relaxation using techniques such as tissue Doppler imaging and speckle-tracking echocardiography, which measure early diastolic velocity and strain rates. Inotropic function is assessed through parameters like ejection fraction, ventricular pressure-volume loops, and myocardial contractility indices obtained via echocardiography, cardiac MRI, or invasive hemodynamic monitoring. Advanced diagnostic tools enable differentiation between impaired relaxation (lusitropy) and reduced contractility (inotropy), facilitating precise clinical management of cardiac dysfunction.
Future Perspectives in Cardiac Therapy: Targeting Lusitropy and Inotropy
Future perspectives in cardiac therapy emphasize precise modulation of lusitropy and inotropy to optimize heart function in heart failure patients. Emerging treatments targeting calcium handling proteins and sarcomeric function show promise in enhancing myocardial relaxation (lusitropy) and contraction strength (inotropy) with minimized adverse effects. Advances in gene editing and molecular therapies aim to selectively adjust these parameters, offering personalized cardiac care and improved patient outcomes.
Lusitropic Infographic
 libterm.com
libterm.com