Meningitis is a serious inflammation of the protective membranes covering the brain and spinal cord, often caused by infections from viruses or bacteria. Early diagnosis and treatment are crucial to prevent severe complications or long-term damage. Discover more about the symptoms, causes, and prevention strategies to protect your health by reading the rest of the article.
Table of Comparison
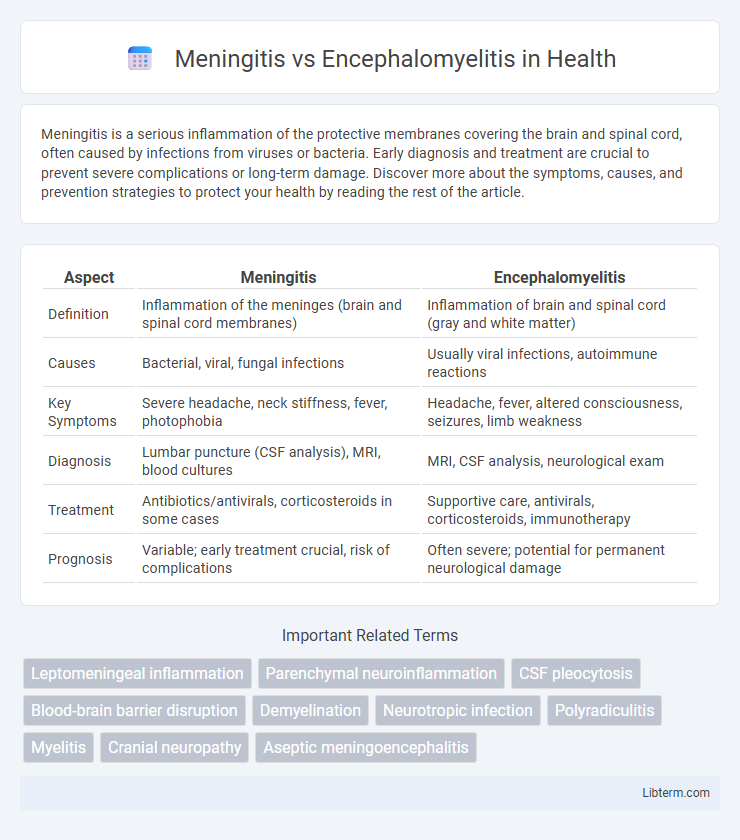
| Aspect | Meningitis | Encephalomyelitis |
|---|---|---|
| Definition | Inflammation of the meninges (brain and spinal cord membranes) | Inflammation of brain and spinal cord (gray and white matter) |
| Causes | Bacterial, viral, fungal infections | Usually viral infections, autoimmune reactions |
| Key Symptoms | Severe headache, neck stiffness, fever, photophobia | Headache, fever, altered consciousness, seizures, limb weakness |
| Diagnosis | Lumbar puncture (CSF analysis), MRI, blood cultures | MRI, CSF analysis, neurological exam |
| Treatment | Antibiotics/antivirals, corticosteroids in some cases | Supportive care, antivirals, corticosteroids, immunotherapy |
| Prognosis | Variable; early treatment crucial, risk of complications | Often severe; potential for permanent neurological damage |
Introduction to Meningitis and Encephalomyelitis
Meningitis is an inflammation of the protective membranes covering the brain and spinal cord, primarily caused by bacterial or viral infections, leading to symptoms such as headache, fever, and neck stiffness. Encephalomyelitis involves inflammation of the brain and spinal cord tissue itself, often resulting from autoimmune reactions or viral infections, and is characterized by neurological deficits and altered mental status. Both conditions require prompt diagnosis and treatment to prevent severe complications and long-term neurological damage.
Definitions and Core Differences
Meningitis is the inflammation of the protective membranes covering the brain and spinal cord, primarily caused by bacterial or viral infections, while encephalomyelitis refers to inflammation of both the brain and spinal cord tissue, often due to autoimmune or infectious processes. The core difference lies in the affected areas: meningitis impacts the meninges, whereas encephalomyelitis involves the neural parenchyma, leading to distinct clinical manifestations and treatment approaches. Diagnostic imaging and cerebrospinal fluid analysis are crucial in differentiating these conditions based on their pathophysiology and etiology.
Causes and Risk Factors
Meningitis is primarily caused by bacterial, viral, or fungal infections that lead to inflammation of the protective membranes surrounding the brain and spinal cord, with risk factors including age, weakened immune system, and close living conditions. Encephalomyelitis is most commonly triggered by viral infections such as herpes simplex virus or autoimmune responses, causing inflammation of both the brain and spinal cord, with risk factors including prior infections, autoimmune diseases, and genetic predisposition. Understanding these distinct causes and risk factors aids in accurate diagnosis and targeted treatment of these central nervous system disorders.
Signs and Symptoms Comparison
Meningitis primarily presents with severe headache, neck stiffness, fever, and photophobia, indicating inflammation of the meninges surrounding the brain and spinal cord. Encephalomyelitis often manifests with altered mental status, seizures, focal neurological deficits, and muscle weakness, reflecting inflammation of both the brain parenchyma and spinal cord. While both conditions may share fever and headache, encephalomyelitis typically includes cognitive impairments and motor dysfunction not commonly seen in meningitis.
Diagnostic Approaches
Meningitis diagnosis primarily involves cerebrospinal fluid (CSF) analysis through lumbar puncture, revealing elevated white blood cells, protein, and decreased glucose levels, alongside blood cultures and polymerase chain reaction (PCR) tests to identify bacterial or viral pathogens. Encephalomyelitis diagnosis requires magnetic resonance imaging (MRI) to detect inflammation in the brain and spinal cord, combined with CSF analysis showing lymphocytic pleocytosis and elevated protein, and autoantibody testing to identify autoimmune causes. Electroencephalography (EEG) may assist in encephalomyelitis by detecting diffuse brain dysfunction, distinguishing it from meningitis, which typically lacks such EEG abnormalities.
Key Differences in Treatment Strategies
Meningitis treatment primarily involves high-dose intravenous antibiotics or antiviral agents targeting bacterial or viral pathogens, alongside corticosteroids to reduce inflammation. Encephalomyelitis management centers on immunosuppressive therapies such as corticosteroids, intravenous immunoglobulin (IVIG), or plasmapheresis to modulate autoimmune responses. Precise diagnosis using cerebrospinal fluid analysis and neuroimaging guides tailored treatment approaches, differentiating infectious meningitis from inflammatory encephalomyelitis.
Prognosis and Potential Complications
Meningitis prognosis varies depending on the pathogen, with bacterial meningitis showing higher mortality and risk of neurological damage compared to viral forms, which often resolve without long-term effects. Encephalomyelitis, particularly acute disseminated encephalomyelitis (ADEM), presents a more unpredictable course, potentially causing lasting cognitive deficits, motor impairment, or seizures due to widespread inflammation of the brain and spinal cord. Both conditions carry risks of complications such as brain swelling, seizures, and permanent neurological disability, but encephalomyelitis generally has a more severe impact on functional recovery.
Prevention and Vaccination
Prevention of meningitis primarily relies on vaccination against common bacterial causes such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b (Hib), which significantly reduce the incidence of bacterial meningitis. Encephalomyelitis prevention focuses on vaccination for viruses like measles, mumps, rubella, and varicella-zoster, aiming to lower the risk of viral infections that can lead to inflammation of the brain and spinal cord. Maintaining up-to-date immunizations and practicing good hygiene are critical public health strategies to control the spread of both meningitis and encephalomyelitis.
Meningitis vs Encephalomyelitis in Children and Adults
Meningitis and encephalomyelitis both involve inflammation of the central nervous system but affect different regions, with meningitis targeting the meninges and encephalomyelitis impacting the brain and spinal cord. In children, bacterial meningitis often presents rapidly with fever, neck stiffness, and altered consciousness, whereas encephalomyelitis typically manifests with neurological deficits, seizures, and behavioral changes. Adults with meningitis experience similar symptoms but have a higher risk of complications, while encephalomyelitis in adults may lead to prolonged cognitive impairment and motor dysfunction depending on the extent of neural inflammation.
When to Seek Medical Attention
Seek immediate medical attention if symptoms such as high fever, severe headache, stiff neck, confusion, or seizures appear, as these may indicate meningitis or encephalomyelitis. Rapid diagnosis and treatment are crucial to prevent complications like brain damage or death. Early intervention with antibiotics or antiviral medications significantly improves outcomes in both conditions.
Meningitis Infographic
 libterm.com
libterm.com