Pharmacokinetics explores how drugs are absorbed, distributed, metabolized, and excreted in the body, influencing their therapeutic effects and potential side effects. Understanding these processes helps optimize drug dosing and timing for maximum efficacy and safety. Discover more about how pharmacokinetics impacts your treatment effectiveness in the rest of this article.
Table of Comparison
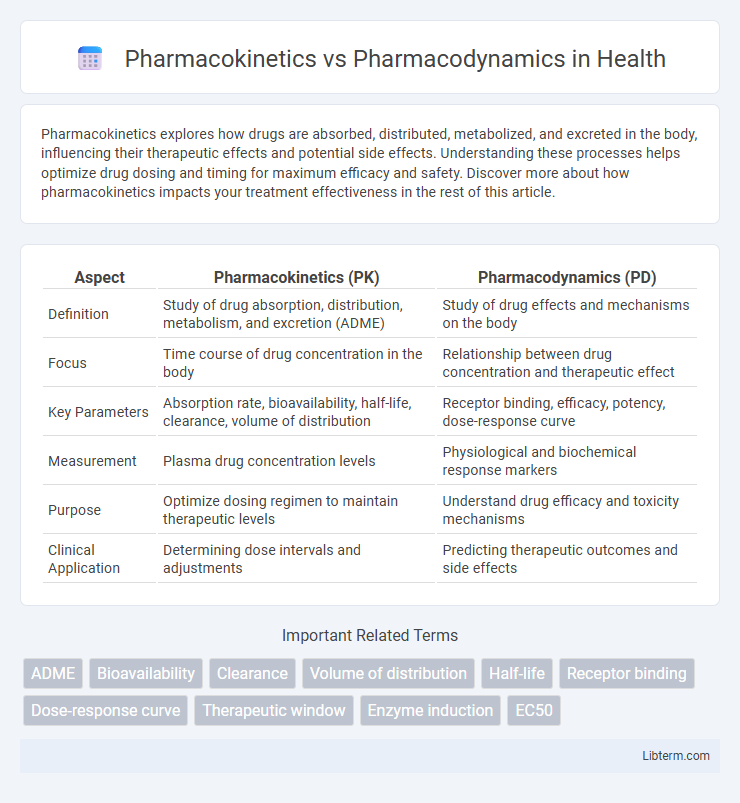
| Aspect | Pharmacokinetics (PK) | Pharmacodynamics (PD) |
|---|---|---|
| Definition | Study of drug absorption, distribution, metabolism, and excretion (ADME) | Study of drug effects and mechanisms on the body |
| Focus | Time course of drug concentration in the body | Relationship between drug concentration and therapeutic effect |
| Key Parameters | Absorption rate, bioavailability, half-life, clearance, volume of distribution | Receptor binding, efficacy, potency, dose-response curve |
| Measurement | Plasma drug concentration levels | Physiological and biochemical response markers |
| Purpose | Optimize dosing regimen to maintain therapeutic levels | Understand drug efficacy and toxicity mechanisms |
| Clinical Application | Determining dose intervals and adjustments | Predicting therapeutic outcomes and side effects |
Introduction to Pharmacokinetics and Pharmacodynamics
Pharmacokinetics describes the absorption, distribution, metabolism, and excretion (ADME) of drugs, detailing how the body processes medication over time. Pharmacodynamics focuses on the biochemical and physiological effects of drugs, including receptor interactions, dose-response relationships, and mechanisms of action. Understanding both pharmacokinetics and pharmacodynamics is essential for optimizing drug efficacy and minimizing toxicity in therapeutic treatments.
Defining Pharmacokinetics: The Journey of Drugs in the Body
Pharmacokinetics describes the dynamic process encompassing absorption, distribution, metabolism, and excretion (ADME) of drugs within the body. It determines the drug's concentration at target sites, influencing onset, intensity, and duration of therapeutic effects. Understanding pharmacokinetics is essential for optimizing dosage regimens and minimizing toxicity, thereby enhancing drug efficacy and safety.
Understanding Pharmacodynamics: Drug Effects and Mechanisms
Pharmacodynamics explores how drugs interact with cellular receptors and target molecules to produce therapeutic effects, emphasizing the relationship between drug concentration and effect. Key mechanisms include receptor binding, signal transduction, and dose-response relationships that determine drug efficacy and potency. Understanding these dynamics helps optimize drug dosing and predict potential side effects for personalized treatment.
Key Differences Between Pharmacokinetics and Pharmacodynamics
Pharmacokinetics involves the absorption, distribution, metabolism, and excretion (ADME) of drugs, determining the concentration of a drug in the body over time. Pharmacodynamics studies the biochemical and physiological effects of drugs and their mechanisms of action at target receptors. Key differences include pharmacokinetics focusing on what the body does to the drug, while pharmacodynamics focuses on what the drug does to the body.
Factors Influencing Pharmacokinetics
Pharmacokinetics involves the absorption, distribution, metabolism, and excretion of drugs, determining the drug concentration over time in the body. Key factors influencing pharmacokinetics include age, genetic polymorphisms affecting metabolic enzymes, liver and kidney function, drug formulation, and interactions with other medications. Understanding these variables is essential for optimizing dosing regimens and improving therapeutic outcomes.
Factors Affecting Pharmacodynamic Responses
Pharmacodynamic responses are influenced by factors such as receptor sensitivity, drug-receptor affinity, and the density of receptors on the target cells. Genetic variations and physiological conditions like age, liver function, and disease states also modify the effectiveness and potency of drugs. Understanding these factors aids in predicting drug efficacy and personalizing therapeutic regimens.
Clinical Importance of Pharmacokinetics and Pharmacodynamics
Pharmacokinetics and pharmacodynamics are crucial in optimizing drug therapy by ensuring appropriate dosing and maximizing therapeutic efficacy while minimizing toxicity. Pharmacokinetics involves the absorption, distribution, metabolism, and excretion of drugs, guiding dosage adjustments based on patient-specific factors such as age, kidney function, and liver metabolism. Pharmacodynamics focuses on drug-receptor interactions and the biochemical effects, helping predict therapeutic outcomes and tailor treatments to achieve desired clinical responses.
Pharmacokinetic and Pharmacodynamic Modeling
Pharmacokinetic modeling quantitatively describes drug absorption, distribution, metabolism, and excretion (ADME) processes, enabling prediction of drug concentration-time profiles in biological systems. Pharmacodynamic modeling evaluates the relationship between drug concentration and its pharmacological effect, facilitating dose-response characterization and optimization of therapeutic regimens. Integrating pharmacokinetic and pharmacodynamic models supports precision medicine by predicting drug efficacy and safety through dynamic simulations of drug behavior and response.
Applications in Drug Development and Personalized Medicine
Pharmacokinetics (PK) involves the study of drug absorption, distribution, metabolism, and excretion, providing critical data for optimizing dosage regimens in drug development. Pharmacodynamics (PD) examines the biochemical and physiological effects of drugs and their mechanisms of action, essential for assessing therapeutic efficacy and safety profiles. Integrating PK/PD modeling enhances personalized medicine by tailoring drug treatments based on individual variability in drug response and metabolism.
Conclusion: Integrating Pharmacokinetics and Pharmacodynamics in Therapeutics
Integrating pharmacokinetics and pharmacodynamics enhances therapeutic effectiveness by optimizing drug dosing based on absorption, distribution, metabolism, and excretion profiles alongside drug-receptor interactions and physiological effects. This synergy supports personalized medicine, improving efficacy while minimizing adverse effects through precise drug concentration and response monitoring. Advances in modeling and simulation further enable prediction of individual patient outcomes, guiding tailored treatment strategies.
Pharmacokinetics Infographic
 libterm.com
libterm.com