Bronchodilation is the process of relaxing the smooth muscles surrounding the airways, leading to their widening and improved airflow to the lungs. This mechanism plays a crucial role in managing respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD). Explore the rest of the article to understand how bronchodilation can benefit Your respiratory health and the treatments involved.
Table of Comparison
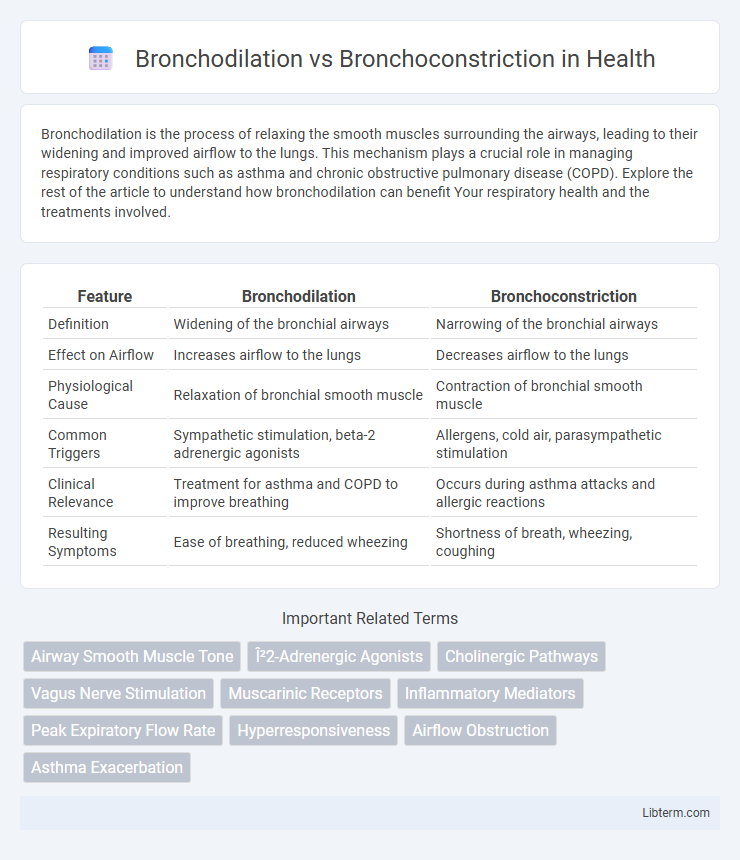
| Feature | Bronchodilation | Bronchoconstriction |
|---|---|---|
| Definition | Widening of the bronchial airways | Narrowing of the bronchial airways |
| Effect on Airflow | Increases airflow to the lungs | Decreases airflow to the lungs |
| Physiological Cause | Relaxation of bronchial smooth muscle | Contraction of bronchial smooth muscle |
| Common Triggers | Sympathetic stimulation, beta-2 adrenergic agonists | Allergens, cold air, parasympathetic stimulation |
| Clinical Relevance | Treatment for asthma and COPD to improve breathing | Occurs during asthma attacks and allergic reactions |
| Resulting Symptoms | Ease of breathing, reduced wheezing | Shortness of breath, wheezing, coughing |
Understanding Bronchodilation and Bronchoconstriction
Bronchodilation refers to the widening of the bronchial airways caused by relaxation of the smooth muscles, which enhances airflow to the lungs and improves oxygen exchange. Bronchoconstriction involves the narrowing of these airways due to muscle contraction, often triggered by allergens, irritants, or inflammatory mediators, leading to restricted airflow and breathing difficulties. Understanding the mechanisms of bronchial smooth muscle regulation is essential for managing respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD).
Mechanisms of Airway Regulation
Bronchodilation occurs when smooth muscle in the airway walls relaxes, typically triggered by sympathetic nervous system activation through beta-2 adrenergic receptors, increasing airway diameter and airflow. Bronchoconstriction involves the contraction of airway smooth muscle caused by parasympathetic stimulation via muscarinic receptors or inflammatory mediators like histamine and leukotrienes, leading to narrowed airways and reduced airflow. The balance between these mechanisms regulates airway resistance and ventilation efficiency in response to physiological demands or pathological conditions such as asthma.
Causes of Bronchodilation
Bronchodilation occurs when the smooth muscles surrounding the airways relax, leading to an increase in airway diameter and improved airflow. It is primarily caused by the activation of beta-2 adrenergic receptors through agents such as epinephrine, certain medications including albuterol, and natural stimuli like sympathetic nervous system activation during physical exertion. Other factors inducing bronchodilation include exposure to mild cold air, certain inhaled corticosteroids, and the reduction of parasympathetic nervous system influence on the lungs.
Triggers of Bronchoconstriction
Bronchoconstriction is primarily triggered by allergens, cold air, exercise, respiratory infections, and exposure to irritants such as smoke or pollution. These stimuli activate the parasympathetic nervous system, causing contraction of the smooth muscle in the airways and narrowing of bronchial passages. In contrast, bronchodilation involves relaxation of these muscles, often induced by beta-2 adrenergic agonists, improving airflow and easing breathing.
Physiological Impact on Respiratory Function
Bronchodilation expands the airways by relaxing bronchial smooth muscle, enhancing airflow and improving oxygen delivery to the lungs. Bronchoconstriction narrows the airways due to muscle contraction, increasing airway resistance and reducing ventilation efficiency. These opposing processes critically regulate respiratory function by controlling airway diameter and gas exchange capacity.
Symptoms Associated with Each Condition
Bronchodilation is characterized by the expansion of bronchial airways, leading to symptoms such as improved airflow, reduced wheezing, and easier breathing, commonly observed during asthma relief or physical exertion. In contrast, bronchoconstriction involves the narrowing of these airways, causing symptoms like shortness of breath, chest tightness, coughing, and wheezing, often triggered by allergens, infections, or chronic respiratory conditions like asthma and chronic obstructive pulmonary disease (COPD). Understanding these symptom patterns is crucial for accurate diagnosis and effective management of respiratory disorders.
Common Disorders Involving Airway Changes
Bronchodilation occurs when the smooth muscles of the airways relax, increasing airflow, whereas bronchoconstriction involves the tightening of these muscles, reducing airway diameter. Common disorders involving these airway changes include asthma, characterized by episodes of bronchoconstriction leading to wheezing and shortness of breath, and chronic obstructive pulmonary disease (COPD), where bronchoconstriction and inflammation cause persistent airflow limitation. Treatment strategies for these disorders often target bronchodilation through beta-agonists or anticholinergic medications to improve breathing and reduce airway resistance.
Diagnostic Approaches for Airway Assessment
Diagnostic approaches for airway assessment differentiate bronchodilation and bronchoconstriction primarily through spirometry, measuring changes in forced expiratory volume (FEV1) before and after bronchodilator administration. Bronchoprovocation tests, such as methacholine challenge, evaluate airway hyperresponsiveness by inducing bronchoconstriction and monitoring lung function decline. Imaging techniques like high-resolution CT scans assist in visualizing airway wall thickening and luminal changes associated with bronchoconstriction, supporting diagnosis and treatment planning.
Treatment Strategies: Dilators vs. Constrictors
Bronchodilation involves the relaxation of bronchial smooth muscle to widen airways, commonly treated with bronchodilators such as beta-2 agonists and anticholinergics that improve airflow in conditions like asthma and COPD. Bronchoconstriction, characterized by airway narrowing due to smooth muscle contraction and inflammation, is managed by avoiding triggers and using anti-inflammatory agents rather than constrictors, as inducing constriction is generally harmful. Treatment strategies focus on enhancing bronchodilation to relieve symptoms and improve lung function while preventing bronchoconstriction through pharmacological and lifestyle interventions.
Prevention and Lifestyle Recommendations
Effective prevention of bronchoconstriction involves avoiding triggers such as allergens, tobacco smoke, and air pollution, while regular use of prescribed bronchodilators helps maintain airway openness. Incorporating breathing exercises, maintaining a healthy weight, and engaging in moderate physical activity contribute to improved lung function and reduce episodes of bronchial narrowing. Consistent medical monitoring and adherence to asthma or COPD action plans optimize bronchodilation and lower the risk of respiratory complications.
Bronchodilation Infographic
 libterm.com
libterm.com