Cycloplegia is a condition characterized by the paralysis of the ciliary muscle of the eye, resulting in loss of accommodation and difficulty focusing on close objects. It is commonly induced for diagnostic purposes in eye exams or during treatment of various ocular conditions to relax the eye muscles and prevent spasms. Discover how cycloplegia affects your vision and why it plays a crucial role in eye care by reading the rest of this article.
Table of Comparison
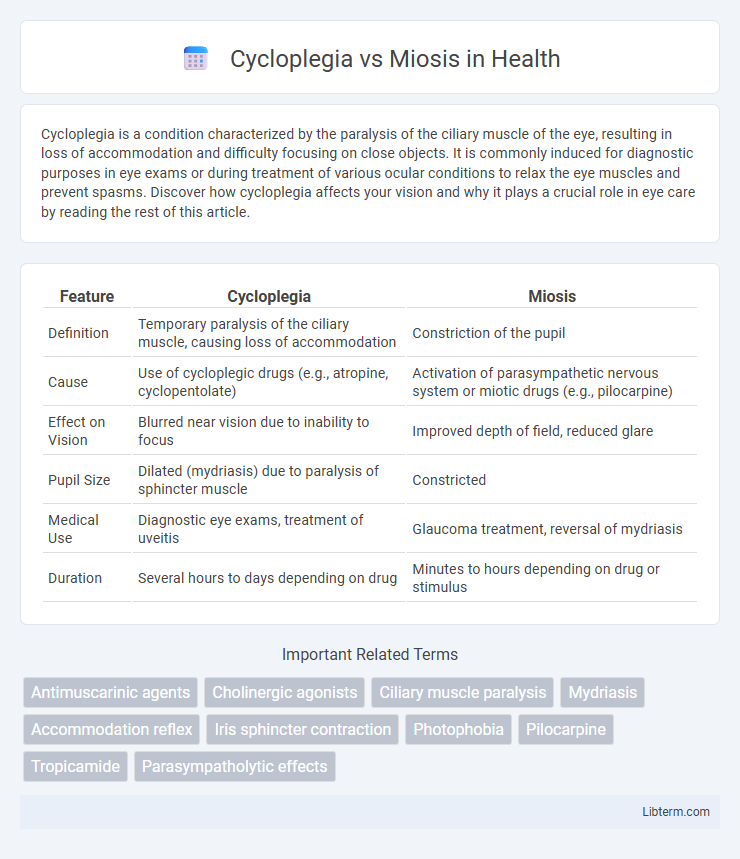
| Feature | Cycloplegia | Miosis |
|---|---|---|
| Definition | Temporary paralysis of the ciliary muscle, causing loss of accommodation | Constriction of the pupil |
| Cause | Use of cycloplegic drugs (e.g., atropine, cyclopentolate) | Activation of parasympathetic nervous system or miotic drugs (e.g., pilocarpine) |
| Effect on Vision | Blurred near vision due to inability to focus | Improved depth of field, reduced glare |
| Pupil Size | Dilated (mydriasis) due to paralysis of sphincter muscle | Constricted |
| Medical Use | Diagnostic eye exams, treatment of uveitis | Glaucoma treatment, reversal of mydriasis |
| Duration | Several hours to days depending on drug | Minutes to hours depending on drug or stimulus |
Introduction to Cycloplegia and Miosis
Cycloplegia is a condition characterized by the paralysis of the ciliary muscle of the eye, leading to loss of accommodation and inability to focus on near objects. Miosis refers to the excessive constriction of the pupil, commonly caused by parasympathetic stimulation affecting the iris sphincter muscle. Both cycloplegia and miosis impact ocular function but affect different muscles and mechanisms within the eye.
Definitions and Basic Concepts
Cycloplegia refers to the paralysis of the ciliary muscle of the eye, resulting in a loss of accommodation and an inability to focus on near objects. Miosis is the constriction of the pupil caused by the contraction of the sphincter pupillae muscle, often triggered by parasympathetic stimulation. Both conditions affect ocular function but involve different muscles and physiological responses within the eye.
Mechanisms of Action
Cycloplegia results from the inhibition of the ciliary muscle by blocking the muscarinic receptors, leading to a loss of accommodation and paralysis of the eye's focusing ability. Miosis, on the other hand, is caused by the stimulation of the sphincter pupillae muscle via muscarinic receptors, resulting in pupil constriction. The primary difference lies in the target muscle and whether muscarinic receptors are antagonized in cycloplegia or agonized in miosis.
Causes and Inducers
Cycloplegia occurs due to paralysis of the ciliary muscle, commonly induced by anticholinergic drugs such as atropine and tropicamide, which inhibit parasympathetic stimulation. Miosis results from constriction of the pupil, typically caused by parasympathomimetic agents like pilocarpine or opioid use, enhancing parasympathetic tone on the sphincter pupillae. Understanding these mechanisms aids in clinical differentiation and targeted treatment of ocular conditions.
Clinical Significance
Cycloplegia is the paralysis of the ciliary muscle, resulting in loss of accommodation and is clinically significant for accurate refractive assessments and treatment of uveitis. Miosis refers to excessive constriction of the pupil, which can indicate pathological conditions such as Horner's syndrome, opioid intoxication, or response to certain medications. Understanding the distinction aids in diagnosing neurological disorders and managing ocular pharmacology effectively.
Diagnostic Applications
Cycloplegia, characterized by the paralysis of the ciliary muscle resulting in loss of accommodation, is primarily used in diagnostic applications to accurately measure refractive errors and uncover latent hyperopia during eye examinations. Miosis, the constriction of the pupil, aids in diagnosing neurological conditions by assessing parasympathetic nervous system function and can help in detecting acute angle-closure glaucoma through pupil behavior analysis. Both cycloplegia and miosis are integral to ophthalmologic diagnostics, providing critical insights into ocular health and systemic neurological status.
Therapeutic Uses
Cycloplegia is primarily used in ophthalmology to relax the ciliary muscle, facilitating accurate refraction assessments and treating uveitis by reducing pain and preventing synechiae formation. Miosis, often induced pharmaceutically by agents like pilocarpine, helps manage glaucoma by increasing aqueous humor outflow and lowering intraocular pressure. Both therapeutic approaches target different ocular conditions, with cycloplegics aiding diagnostic and inflammatory control, while miotics focus on glaucoma treatment and enhancing pupil constriction.
Side Effects and Risks
Cycloplegia causes temporary paralysis of the ciliary muscle, leading to blurred vision, photophobia, and difficulty focusing on near objects, with risks including increased intraocular pressure and potential angle-closure glaucoma. Miosis, the excessive constriction of the pupil, can result in decreased night vision, headaches, and eye pain, with risks such as impaired vision in low-light conditions and exacerbation of pre-existing eye diseases. Both conditions require careful monitoring to avoid complications, especially in patients with glaucoma or inflammatory eye disorders.
Comparative Analysis: Cycloplegia vs Miosis
Cycloplegia involves paralysis of the ciliary muscle, resulting in loss of accommodation and pupil dilation, whereas miosis refers to the constriction of the pupil due to sphincter muscle contraction. Cycloplegia is commonly induced by anticholinergic agents like atropine to facilitate eye examinations, while miosis occurs naturally in response to bright light or parasympathetic stimulation. The functional distinction lies in cycloplegia impairing near vision and accommodation, contrasting with miosis enhancing depth of field and reducing light entry.
Future Perspectives in Ophthalmology
Emerging therapies in ophthalmology aim to selectively modulate cycloplegia and miosis to enhance diagnostic precision and treatment outcomes for conditions like uveitis and glaucoma. Advances in gene therapy and targeted drug delivery promise to minimize side effects while maximizing the control over pupillary responses. Ongoing research into biometric feedback integration may enable personalized ocular pharmacology, improving both cycloplegic and miotic agent efficacy in clinical practice.
Cycloplegia Infographic
 libterm.com
libterm.com