Gout and cellulitis are distinct conditions that can cause severe inflammation and pain, often affecting the skin and joints. Identifying the differences in symptoms and treatment is crucial for effective management and avoiding complications. Discover how to differentiate between these disorders and what steps you should take to protect your health in the rest of the article.
Table of Comparison
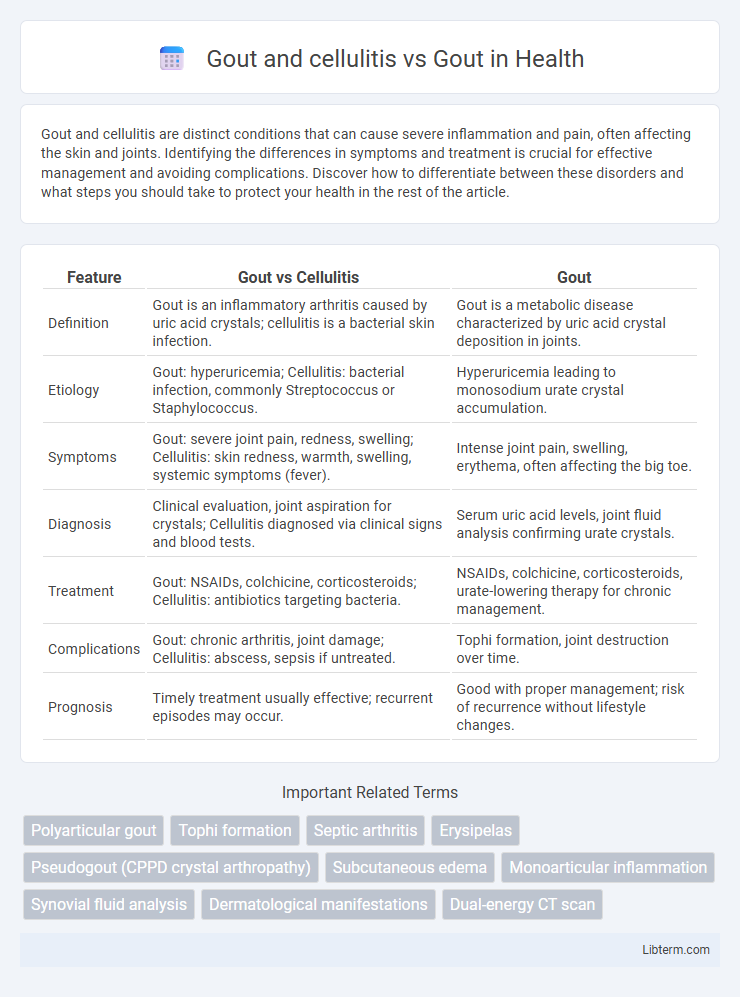
| Feature | Gout vs Cellulitis | Gout |
|---|---|---|
| Definition | Gout is an inflammatory arthritis caused by uric acid crystals; cellulitis is a bacterial skin infection. | Gout is a metabolic disease characterized by uric acid crystal deposition in joints. |
| Etiology | Gout: hyperuricemia; Cellulitis: bacterial infection, commonly Streptococcus or Staphylococcus. | Hyperuricemia leading to monosodium urate crystal accumulation. |
| Symptoms | Gout: severe joint pain, redness, swelling; Cellulitis: skin redness, warmth, swelling, systemic symptoms (fever). | Intense joint pain, swelling, erythema, often affecting the big toe. |
| Diagnosis | Clinical evaluation, joint aspiration for crystals; Cellulitis diagnosed via clinical signs and blood tests. | Serum uric acid levels, joint fluid analysis confirming urate crystals. |
| Treatment | Gout: NSAIDs, colchicine, corticosteroids; Cellulitis: antibiotics targeting bacteria. | NSAIDs, colchicine, corticosteroids, urate-lowering therapy for chronic management. |
| Complications | Gout: chronic arthritis, joint damage; Cellulitis: abscess, sepsis if untreated. | Tophi formation, joint destruction over time. |
| Prognosis | Timely treatment usually effective; recurrent episodes may occur. | Good with proper management; risk of recurrence without lifestyle changes. |
Understanding Gout: Causes and Symptoms
Gout is a form of arthritis characterized by sudden, severe attacks of pain, redness, and swelling due to urate crystal accumulation in joints, most commonly affecting the big toe. Differentiating gout from cellulitis is crucial, as cellulitis is a bacterial skin infection presenting with warmth, redness, and swelling but typically involving systemic symptoms like fever. Understanding the distinct causes--hyperuricemia for gout and bacterial infection for cellulitis--enables accurate diagnosis and effective treatment planning.
What is Cellulitis? Key Features and Risk Factors
Cellulitis is a bacterial skin infection characterized by redness, swelling, warmth, and pain, often caused by Streptococcus or Staphylococcus bacteria. Key features include rapid onset of symptoms, fever, and possible lymphangitis, distinguishing it from gout, which involves joint inflammation due to uric acid crystal deposition. Risk factors for cellulitis include skin trauma, immune suppression, diabetes, and chronic edema, whereas gout primarily relates to hyperuricemia and metabolic syndrome.
Gout vs. Cellulitis: Similarities and Differences
Gout and cellulitis both cause redness, swelling, and pain in affected tissues, often leading to misdiagnosis due to overlapping symptoms. Gout is a metabolic disorder characterized by uric acid crystal deposition primarily in joints, while cellulitis is a bacterial skin infection caused most commonly by Streptococcus or Staphylococcus species. Unlike cellulitis, which typically responds to antibiotics, gout treatment focuses on lowering uric acid levels and managing inflammation with NSAIDs or corticosteroids.
Recognizing Overlapping Symptoms
Gout and cellulitis share overlapping symptoms such as intense joint pain, swelling, redness, and warmth, complicating accurate diagnosis. Differentiating factors include the presence of systemic infection signs like fever and lymphangitis in cellulitis, whereas gout typically involves recurrent episodes of acute monoarticular arthritis with hyperuricemia. Early recognition of these overlapping symptoms is crucial for appropriate treatment to prevent mismanagement and potential complications.
How Gout Complicates Cellulitis Diagnosis
Gout often mimics cellulitis by causing intense joint inflammation, redness, and swelling, which can obscure the accurate diagnosis of cellulitis. This overlap in symptoms leads to challenges in distinguishing between the crystal-induced arthritis of gout and the bacterial skin infection characteristic of cellulitis. Timely differentiation using joint fluid analysis and clinical history is essential to avoid misdiagnosis and ensure appropriate treatment.
Diagnostic Techniques: Differentiating Gout from Cellulitis
Differentiating gout from cellulitis relies heavily on diagnostic techniques such as synovial fluid analysis, where urate crystals confirm gout, while cellulitis shows elevated white blood cells indicative of bacterial infection. Imaging methods like ultrasound can detect joint inflammation and tophi specific to gout, whereas cellulitis typically presents with diffuse soft tissue swelling and erythema without joint involvement. Blood tests measuring serum uric acid help support gout diagnosis, but elevated inflammatory markers like C-reactive protein and white blood cell count are more pronounced in cellulitis.
Treatment Approaches for Gout Alone
Treatment approaches for gout primarily involve the use of nonsteroidal anti-inflammatory drugs (NSAIDs), colchicine, and corticosteroids to reduce acute inflammation and manage pain. Long-term management includes urate-lowering therapy such as allopurinol or febuxostat to maintain serum uric acid levels below 6 mg/dL, preventing future flare-ups and joint damage. Lifestyle modifications, including dietary changes to reduce purine intake, weight management, and alcohol reduction, play a crucial role in complementing pharmaceutical interventions for effective gout control.
Managing Gout with Concurrent Cellulitis
Managing gout with concurrent cellulitis requires precise anti-inflammatory treatment while addressing the bacterial infection with appropriate antibiotics. Close monitoring of uric acid levels and inflammatory markers helps prevent exacerbation of gout symptoms during cellulitis therapy. Coordinated care between rheumatologists and infectious disease specialists optimizes patient outcomes by balancing urate-lowering strategies with infection control.
Long-Term Complications: Joint Damage and Infections
Gout causes long-term complications primarily through repeated joint inflammation leading to chronic joint damage, including tophi formation and bone erosion. Cellulitis, often concurrent with gout due to skin infections in compromised tissue, increases the risk of severe infections and systemic spread but does not directly cause joint damage. Effective management of gout focuses on controlling uric acid levels to prevent joint destruction, while preventing cellulitis requires prompt antibiotic treatment to avoid life-threatening infections.
Prevention Tips for Gout and Cellulitis
Proper hydration and a low-purine diet significantly reduce the risk of gout flare-ups by preventing uric acid crystal formation. Maintaining skin hygiene and promptly treating wounds minimize the chance of developing cellulitis, especially in individuals prone to gout-related joint swelling. Regular exercise and weight management lower inflammation and improve immune function, supporting prevention of both gout attacks and cellulitis infections.
Gout and cellulitis Infographic
 libterm.com
libterm.com