Neutropenia and anemia are common blood disorders characterized by a decrease in white blood cells and red blood cells, respectively, leading to increased infection risk and fatigue. Understanding the causes, symptoms, and treatment options is crucial for managing your health effectively. Explore the full article to learn how to identify and address these conditions.
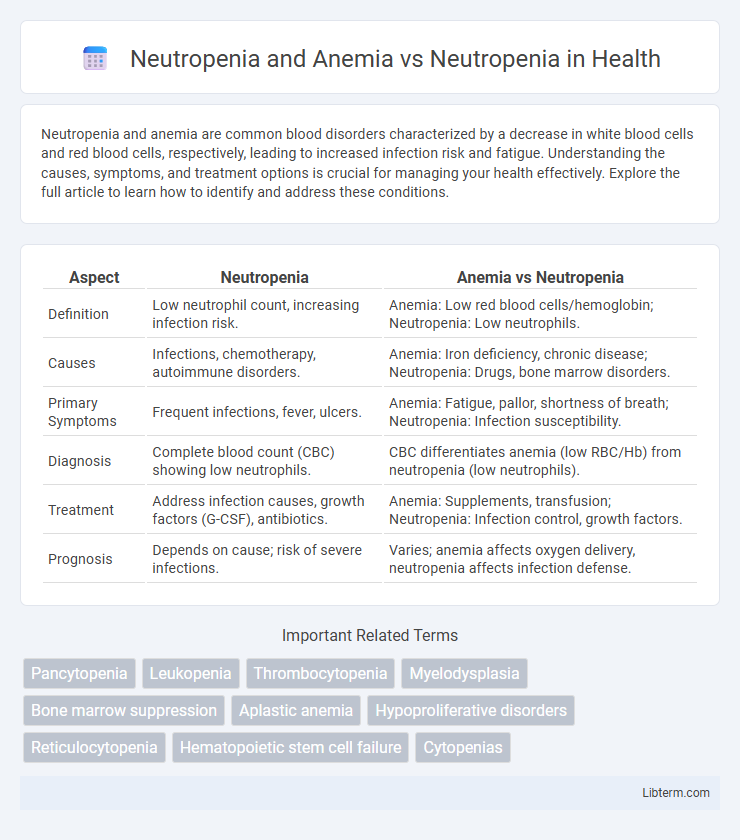
Table of Comparison
| Aspect | Neutropenia | Anemia vs Neutropenia |
|---|---|---|
| Definition | Low neutrophil count, increasing infection risk. | Anemia: Low red blood cells/hemoglobin; Neutropenia: Low neutrophils. |
| Causes | Infections, chemotherapy, autoimmune disorders. | Anemia: Iron deficiency, chronic disease; Neutropenia: Drugs, bone marrow disorders. |
| Primary Symptoms | Frequent infections, fever, ulcers. | Anemia: Fatigue, pallor, shortness of breath; Neutropenia: Infection susceptibility. |
| Diagnosis | Complete blood count (CBC) showing low neutrophils. | CBC differentiates anemia (low RBC/Hb) from neutropenia (low neutrophils). |
| Treatment | Address infection causes, growth factors (G-CSF), antibiotics. | Anemia: Supplements, transfusion; Neutropenia: Infection control, growth factors. |
| Prognosis | Depends on cause; risk of severe infections. | Varies; anemia affects oxygen delivery, neutropenia affects infection defense. |
Understanding Neutropenia: Causes and Consequences
Neutropenia is characterized by a reduced neutrophil count, increasing susceptibility to bacterial infections due to impaired immune defense. When neutropenia coexists with anemia, patients often experience compounded symptoms such as fatigue, pallor, and heightened infection risk, reflecting both compromised oxygen delivery and immune function. Understanding the etiology of neutropenia includes factors like chemotherapy, bone marrow disorders, and autoimmune diseases, which can disrupt neutrophil production and lifespan.
Defining Anemia: Symptoms and Underlying Mechanisms
Anemia is defined by a decreased number of red blood cells or hemoglobin, leading to reduced oxygen transport and symptoms such as fatigue, pallor, and shortness of breath. Underlying mechanisms of anemia include iron deficiency, chronic disease, or bone marrow suppression, which differ from neutropenia that primarily involves low neutrophil counts affecting immune response. Understanding anemia's pathophysiology is critical for distinguishing its clinical presentation from isolated neutropenia and guiding targeted treatment strategies.
Neutropenia and Anemia: Overlapping Pathophysiology
Neutropenia and anemia frequently coexist due to overlapping pathophysiological mechanisms such as bone marrow suppression, autoimmune destruction, and nutrient deficiencies affecting hematopoiesis. Both conditions share common etiologies including chemotherapy-induced myelosuppression, chronic infections, and marrow infiltration by malignancies, leading to simultaneous reductions in neutrophils and red blood cells. Understanding the intertwined cellular and molecular pathways in neutropenia and anemia enhances diagnostic accuracy and informs targeted therapeutic strategies.
Distinguishing Neutropenia from Combined Neutropenia and Anemia
Neutropenia involves a decreased neutrophil count, increasing infection risk, whereas combined neutropenia and anemia present simultaneous reductions in neutrophils and red blood cells, leading to immunodeficiency alongside oxygen transport impairment. Diagnostic differentiation relies on complete blood count (CBC) analysis, bone marrow biopsy, and reticulocyte count to identify isolated neutrophil depletion versus multi-lineage hematopoietic suppression. Treatment strategies diverge, with neutropenia alone often managed by granulocyte colony-stimulating factor (G-CSF), while combined conditions may require erythropoiesis-stimulating agents and supportive transfusions addressing both cell line deficiencies.
Risk Factors for Isolated Neutropenia
Isolated neutropenia primarily arises from viral infections, autoimmune disorders, and certain medications such as chemotherapeutic agents or antibiotics, while neutropenia combined with anemia often results from bone marrow failure syndromes or nutritional deficiencies like vitamin B12 or folate deficiency. Risk factors for isolated neutropenia include recurrent infections, exposure to toxic chemicals, and genetic predisposition, whereas the presence of anemia alongside neutropenia typically points to broader hematologic conditions. Identifying specific risk factors aids in differential diagnosis and targeted treatment strategies to manage isolated neutropenia effectively.
Clinical Implications of Coexisting Neutropenia and Anemia
Coexisting neutropenia and anemia significantly increase the risk of severe infections and impaired oxygen delivery, complicating clinical management and worsening patient outcomes. The dual hematologic deficits necessitate careful monitoring and often prompt interventions such as growth factor support, transfusions, or antimicrobial prophylaxis to prevent life-threatening complications. Understanding the interplay between these conditions is critical for optimizing treatment strategies and improving prognosis in affected patients.
Diagnostic Approaches: Neutropenia Alone versus Dual Cytopenias
Diagnostic approaches for neutropenia alone typically involve complete blood count (CBC) with differential, peripheral blood smear, and assessment of bone marrow function to identify causes such as infections or drug-induced suppression. In cases of dual cytopenias, including neutropenia and anemia, evaluation extends to bone marrow biopsy and cytogenetic analysis to detect underlying hematologic disorders like myelodysplastic syndromes or marrow infiltration. Comprehensive diagnostic strategies enhance differentiation between isolated neutropenia and complex marrow pathologies, guiding targeted treatment.
Treatment Strategies: Tailoring Therapy for Single vs Combined Conditions
Treatment strategies for neutropenia alone typically focus on addressing the underlying cause and may include growth factors like G-CSF to stimulate neutrophil production, alongside infection prevention measures. In cases where neutropenia is combined with anemia, therapy must be more nuanced, incorporating treatments targeting both conditions such as erythropoiesis-stimulating agents for anemia and immunosuppressive therapy if myelodysplastic syndromes or bone marrow failure are involved. Personalized treatment plans based on the severity and etiology of each condition improve patient outcomes by effectively managing hematopoietic deficits and minimizing complications.
Prognosis and Outcomes: Isolated Neutropenia vs Combined Blood Disorders
Isolated neutropenia generally presents a more favorable prognosis with lower risks of complications and better overall survival compared to combined blood disorders involving anemia and neutropenia. Patients with concurrent anemia and neutropenia often exhibit more severe clinical symptoms, increased susceptibility to infections, and longer hospital stays, leading to a poorer outcome. Early diagnosis and targeted treatment strategies are critical for improving prognosis in combined hematologic abnormalities.
Preventive Measures and Monitoring for At-Risk Populations
Preventive measures for neutropenia and anemia focus on regular blood count monitoring, nutritional support rich in iron, folate, and vitamin B12, and avoiding exposure to infections for at-risk populations such as chemotherapy patients and individuals with autoimmune diseases. Early detection through complete blood count (CBC) tests enables timely intervention with treatments like granulocyte colony-stimulating factor (G-CSF) or erythropoiesis-stimulating agents (ESAs) to reduce complications. Close monitoring ensures management of neutrophil and hemoglobin levels, minimizing the risk of severe infections and fatigue in vulnerable groups.
Neutropenia and Anemia Infographic
 libterm.com
libterm.com