Reactogenicity refers to the physical reaction your body experiences after receiving a vaccine, such as fever, soreness, or fatigue, indicating an inflammatory response. Understanding this concept helps you better anticipate and manage temporary side effects that signify the immune system's activation. Explore the rest of this article to learn how reactogenicity impacts vaccine effectiveness and safety.
Table of Comparison
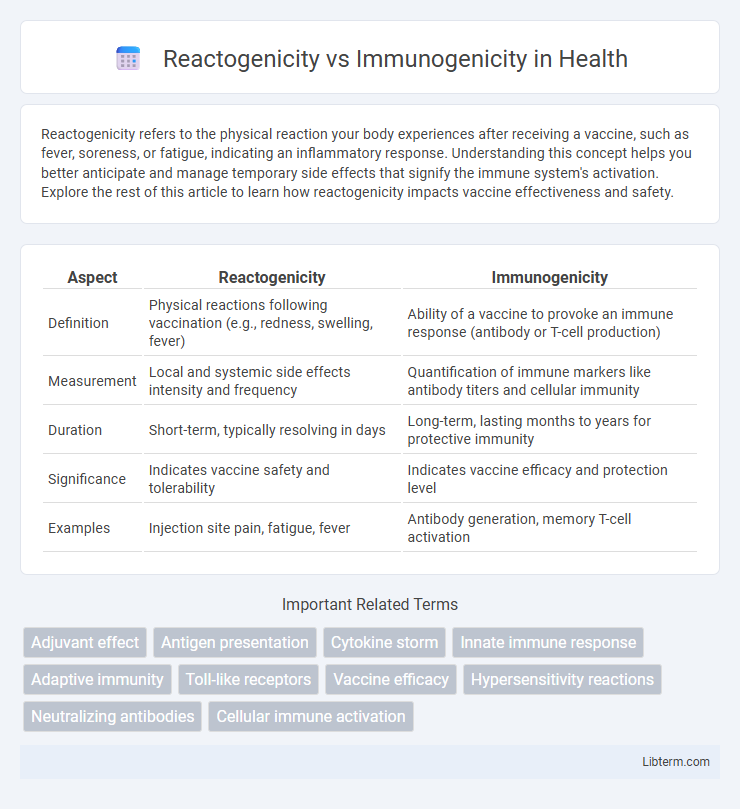
| Aspect | Reactogenicity | Immunogenicity |
|---|---|---|
| Definition | Physical reactions following vaccination (e.g., redness, swelling, fever) | Ability of a vaccine to provoke an immune response (antibody or T-cell production) |
| Measurement | Local and systemic side effects intensity and frequency | Quantification of immune markers like antibody titers and cellular immunity |
| Duration | Short-term, typically resolving in days | Long-term, lasting months to years for protective immunity |
| Significance | Indicates vaccine safety and tolerability | Indicates vaccine efficacy and protection level |
| Examples | Injection site pain, fatigue, fever | Antibody generation, memory T-cell activation |
Understanding Reactogenicity and Immunogenicity
Reactogenicity refers to the physical reactions and side effects that occur soon after vaccination, such as pain, redness, fever, or swelling, indicating the body's initial response to the vaccine. Immunogenicity measures the vaccine's ability to trigger a specific immune response, including antibody production and T-cell activation, essential for long-term protection against infections. Understanding reactogenicity helps assess vaccine safety and tolerability, while evaluating immunogenicity ensures vaccine effectiveness in generating a protective immune barrier.
Defining Reactogenicity: What It Means
Reactogenicity refers to the physical manifestation of the inflammatory response triggered by a vaccine, including symptoms such as pain, redness, swelling at the injection site, fever, and fatigue. It indicates the immediate adverse reactions and local or systemic side effects that result from the innate immune response activation. Understanding reactogenicity is crucial for evaluating vaccine safety profiles and predicting the tolerability of immunization in different populations.
Immunogenicity Explained: The Body’s Immune Response
Immunogenicity refers to the ability of a vaccine or antigen to provoke a robust and specific immune response, characterized by the activation of B cells, T cells, and the production of antibodies. This immune response involves antigen presentation, clonal expansion, and the generation of memory cells, which provide long-lasting protection against pathogens. Measuring immunogenicity is critical in vaccine development to ensure effective immunity without causing excessive reactogenicity, which involves adverse inflammatory reactions.
Key Differences Between Reactogenicity and Immunogenicity
Reactogenicity refers to the physical signs of inflammation and side effects such as pain, redness, or fever occurring shortly after vaccination, while immunogenicity measures the ability of a vaccine to provoke an immune response, including antibody and T-cell production. Reactogenicity is typically a short-term, observable reaction indicating innate immune activation, whereas immunogenicity reflects the long-term effectiveness of the vaccine in establishing immune memory. Understanding the distinction is crucial for vaccine development, balancing safety and efficacy to optimize protective outcomes.
Why Reactogenicity Matters in Vaccine Development
Reactogenicity reflects the short-term side effects triggered by vaccines, such as pain, swelling, and fever, which indicate the body's immediate inflammatory response. Understanding reactogenicity is crucial in vaccine development to balance safety and compliance, ensuring vaccines are well-tolerated to increase public acceptance. High reactogenicity may deter vaccine uptake despite strong immunogenicity, so optimizing reactogenicity profiles helps create effective and patient-friendly vaccines.
The Role of Immunogenicity in Vaccine Effectiveness
Immunogenicity is the key determinant of vaccine effectiveness, reflecting the ability of a vaccine to provoke a robust and lasting immune response against a specific pathogen. High immunogenicity ensures the generation of neutralizing antibodies and memory T cells that provide long-term protection and reduce disease severity. Unlike reactogenicity, which involves transient side effects, immunogenicity directly correlates with the vaccine's protective efficacy and durability against infection.
Measuring Reactogenicity: Common Methods and Metrics
Measuring reactogenicity involves evaluating the physical and systemic responses to vaccination, commonly using metrics such as local injection site reactions, including pain, redness, and swelling, along with systemic symptoms like fever, fatigue, and headache. Standardized tools like patient diaries, visual analog scales (VAS), and clinical grading scales facilitate consistent assessment of reactogenicity severity and duration. Quantitative data on reactogenicity informs vaccine safety profiles and aids in balancing immune response efficacy against tolerability in immunogenicity studies.
Assessing Immunogenicity: Tools and Techniques
Assessing immunogenicity involves measuring the immune system's response to a vaccine or antigen using techniques such as enzyme-linked immunosorbent assay (ELISA), flow cytometry, and neutralization assays. These tools detect specific antibodies, quantify T-cell activation, and evaluate functional immune protection, providing critical data on vaccine efficacy. Accurate immunogenicity assessment distinguishes desired immune responses from adverse reactogenicity effects, guiding vaccine optimization strategies.
Balancing Reactogenicity and Immunogenicity in Vaccines
Balancing reactogenicity and immunogenicity in vaccines requires minimizing adverse reactions while maximizing immune response effectiveness. High reactogenicity can cause temporary side effects but may also correlate with stronger immunogenicity, posing challenges in vaccine formulation. Advances in adjuvant technology and dosing strategies optimize this balance to ensure safety without compromising protective immunity.
Future Perspectives: Innovations in Vaccine Safety and Efficacy
Future perspectives in vaccine development emphasize innovations that enhance immunogenicity while minimizing reactogenicity through advanced platforms like mRNA and nanoparticle vaccines. Precision immunology leveraging AI-driven algorithms enables tailored vaccine formulations that optimize immune responses and reduce adverse effects. Emerging biomarkers and real-time monitoring tools facilitate rapid assessment of vaccine safety profiles, accelerating regulatory approvals and improving public health outcomes.
Reactogenicity Infographic
 libterm.com
libterm.com