Tuberculosis is a contagious bacterial infection primarily affecting the lungs, caused by Mycobacterium tuberculosis. Early detection and appropriate treatment are crucial to prevent severe health complications and curb transmission. Discover more about symptoms, prevention, and treatment options to protect your health throughout the article.
Table of Comparison
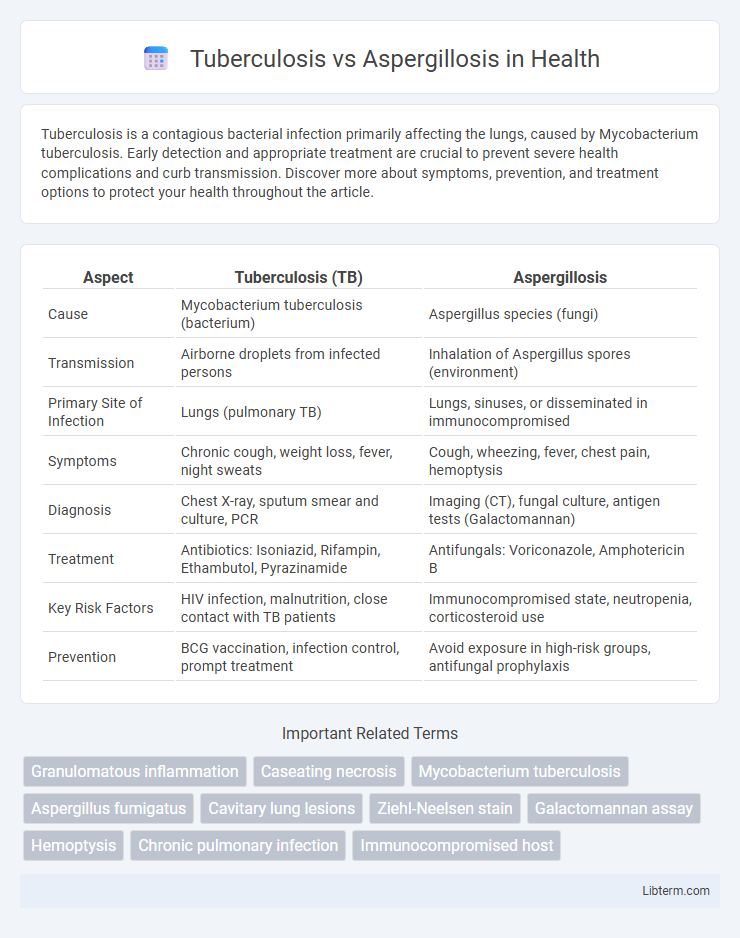
| Aspect | Tuberculosis (TB) | Aspergillosis |
|---|---|---|
| Cause | Mycobacterium tuberculosis (bacterium) | Aspergillus species (fungi) |
| Transmission | Airborne droplets from infected persons | Inhalation of Aspergillus spores (environment) |
| Primary Site of Infection | Lungs (pulmonary TB) | Lungs, sinuses, or disseminated in immunocompromised |
| Symptoms | Chronic cough, weight loss, fever, night sweats | Cough, wheezing, fever, chest pain, hemoptysis |
| Diagnosis | Chest X-ray, sputum smear and culture, PCR | Imaging (CT), fungal culture, antigen tests (Galactomannan) |
| Treatment | Antibiotics: Isoniazid, Rifampin, Ethambutol, Pyrazinamide | Antifungals: Voriconazole, Amphotericin B |
| Key Risk Factors | HIV infection, malnutrition, close contact with TB patients | Immunocompromised state, neutropenia, corticosteroid use |
| Prevention | BCG vaccination, infection control, prompt treatment | Avoid exposure in high-risk groups, antifungal prophylaxis |
Overview of Tuberculosis and Aspergillosis
Tuberculosis (TB) is a contagious bacterial infection caused by Mycobacterium tuberculosis, primarily affecting the lungs and characterized by symptoms like persistent cough, weight loss, and night sweats. Aspergillosis is a fungal infection caused by Aspergillus species, commonly affecting immunocompromised individuals and presenting in forms such as allergic bronchopulmonary aspergillosis, chronic pulmonary aspergillosis, and invasive aspergillosis. Both diseases impact respiratory function but differ fundamentally in etiology, clinical presentation, and treatment approaches.
Causative Agents and Pathogenesis
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis, which primarily infects the lungs by evading immune defenses and forming granulomas. Aspergillosis is caused by Aspergillus species, mainly Aspergillus fumigatus, which produces airborne spores that invade lung tissue and trigger allergic or invasive immune responses. The pathogenesis of tuberculosis involves chronic inflammation and tissue necrosis, whereas aspergillosis pathogenesis ranges from hypersensitivity reactions to angioinvasive disease, especially in immunocompromised hosts.
Modes of Transmission
Tuberculosis primarily spreads through airborne particles expelled when an infected person coughs or sneezes, leading to inhalation of Mycobacterium tuberculosis by others. Aspergillosis is caused by inhaling spores of Aspergillus fungi, which are commonly present in the environment, especially in soil, decaying vegetation, and dust. While tuberculosis requires close contact for transmission, aspergillosis infection occurs mainly through environmental exposure and is more common in immunocompromised individuals.
Clinical Manifestations and Symptoms
Tuberculosis primarily presents with chronic cough, hemoptysis, night sweats, and weight loss, indicating pulmonary involvement, while Aspergillosis often causes wheezing, chest pain, and recurrent hemoptysis, particularly in immunocompromised patients. Both conditions can lead to fever and respiratory distress, but Aspergillosis may show allergic bronchopulmonary reactions or invasive disease features. Radiologic findings differ, with cavitary lesions in Tuberculosis and characteristic nodules or fungal balls in Aspergillosis.
Diagnostic Approaches and Techniques
Diagnostic approaches for Tuberculosis primarily include sputum smear microscopy, culture tests, and nucleic acid amplification tests (NAATs) like the Xpert MTB/RIF assay, which offer high sensitivity and specificity for detecting Mycobacterium tuberculosis. Aspergillosis diagnosis relies heavily on imaging techniques such as high-resolution CT scans to identify characteristic lung lesions, combined with microbiological cultures, galactomannan antigen testing, and PCR assays to detect Aspergillus species. Both infections require integration of clinical, radiological, and laboratory data to differentiate between fungal and mycobacterial pulmonary diseases accurately.
Radiological and Laboratory Findings
Radiological findings in tuberculosis often reveal cavitary lesions, nodules, and upper lobe infiltrates on chest X-rays or CT scans, whereas aspergillosis typically shows halo or air-crescent signs and fungal balls within pre-existing cavities. Laboratory diagnosis of tuberculosis relies on sputum smear microscopy, culture for Mycobacterium tuberculosis, and molecular tests like GeneXpert, while aspergillosis diagnosis includes serum galactomannan antigen detection, Aspergillus-specific IgG antibodies, and fungal cultures. Both infections may require histopathological examination for definitive diagnosis, with acid-fast bacilli for tuberculosis and septate hyphae on tissue biopsy for aspergillosis.
Risk Factors and At-Risk Populations
Tuberculosis primarily affects individuals with weakened immune systems, such as those with HIV/AIDS, malnutrition, or living in crowded, low-income settings. Aspergillosis risk increases in patients with chronic lung diseases, such as cystic fibrosis or COPD, and those undergoing prolonged corticosteroid therapy or chemotherapy. Both infections disproportionately impact immunocompromised populations, but Aspergillosis is particularly prevalent in hospital settings and among transplant recipients.
Treatment Strategies and Medications
Treatment strategies for Tuberculosis primarily involve a prolonged course of first-line antitubercular drugs such as isoniazid, rifampin, ethambutol, and pyrazinamide, often spanning six months to prevent resistance and ensure eradication of Mycobacterium tuberculosis. Aspergillosis management requires antifungal agents like voriconazole or amphotericin B tailored to the disease form, with invasive aspergillosis demanding aggressive therapy and sometimes surgical intervention. Identifying drug resistance patterns and patient immune status is critical for optimizing therapeutic regimens in both infections.
Complications and Prognosis Comparison
Tuberculosis can lead to severe complications such as pulmonary fibrosis, cavitation, and hemoptysis, often resulting in chronic respiratory impairment and a variable prognosis depending on timely diagnosis and treatment adherence. Aspergillosis, particularly invasive forms, may cause life-threatening complications including chronic pulmonary aspergillosis and allergic bronchopulmonary aspergillosis, frequently leading to progressive lung damage and heightened mortality risk in immunocompromised patients. Prognosis for tuberculosis generally improves with appropriate antibiotic therapy, while aspergillosis prognosis depends heavily on immune status and antifungal treatment responsiveness.
Prevention and Public Health Considerations
Effective prevention of tuberculosis (TB) involves widespread Bacillus Calmette-Guerin (BCG) vaccination, early detection through smear microscopy and molecular testing, and ensuring adequate ventilation in crowded settings to reduce airborne transmission. Aspergillosis prevention centers on minimizing exposure to Aspergillus spores by controlling environmental sources such as decaying vegetation and improving indoor air filtration, especially in immunocompromised populations. Public health strategies prioritize TB control programs integrating active case finding, contact tracing, and directly observed therapy (DOT), while aspergillosis prevention relies on surveillance in at-risk patients and environmental management to mitigate fungal outbreaks.
Tuberculosis Infographic
 libterm.com
libterm.com