Osteomalacia and osteoporosis are distinct bone disorders that both result in weakened bones and increased fracture risk, but they differ in cause and pathology. Osteomalacia involves softening of the bones due to defective bone mineralization, often caused by vitamin D deficiency, while osteoporosis is characterized by reduced bone density and structural deterioration. Explore the article to understand how each condition affects your bones and the best approaches for prevention and treatment.
Table of Comparison
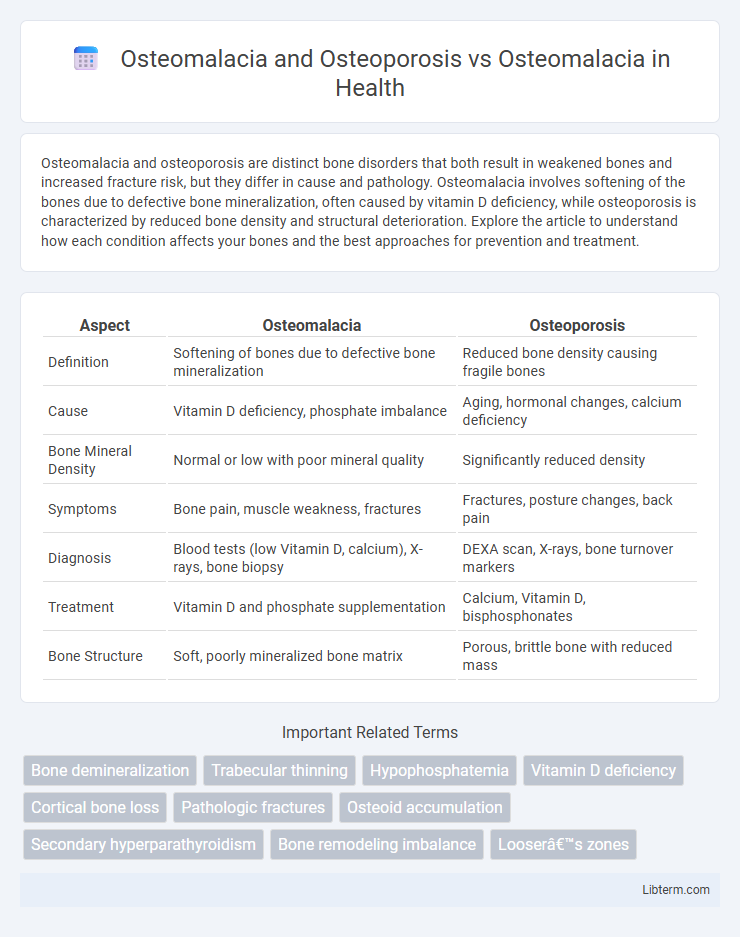
| Aspect | Osteomalacia | Osteoporosis |
|---|---|---|
| Definition | Softening of bones due to defective bone mineralization | Reduced bone density causing fragile bones |
| Cause | Vitamin D deficiency, phosphate imbalance | Aging, hormonal changes, calcium deficiency |
| Bone Mineral Density | Normal or low with poor mineral quality | Significantly reduced density |
| Symptoms | Bone pain, muscle weakness, fractures | Fractures, posture changes, back pain |
| Diagnosis | Blood tests (low Vitamin D, calcium), X-rays, bone biopsy | DEXA scan, X-rays, bone turnover markers |
| Treatment | Vitamin D and phosphate supplementation | Calcium, Vitamin D, bisphosphonates |
| Bone Structure | Soft, poorly mineralized bone matrix | Porous, brittle bone with reduced mass |
Introduction to Osteomalacia
Osteomalacia is a metabolic bone disorder characterized by defective bone mineralization, leading to softening of the bones due to a deficiency of vitamin D or phosphate. Unlike osteoporosis, which involves decreased bone density and increased fracture risk due to bone resorption, osteomalacia primarily results from impaired bone mineralization causing bone pain, muscle weakness, and deformities. Understanding osteomalacia's pathophysiology highlights the critical role of vitamin D metabolism in maintaining skeletal health and differentiates it from osteoporosis in diagnosis and treatment.
Introduction to Osteoporosis
Osteoporosis is a systemic skeletal disorder characterized by decreased bone mass and microarchitectural deterioration, leading to increased fracture risk, commonly affecting postmenopausal women and the elderly. Unlike osteomalacia, which results from defective bone mineralization due to vitamin D deficiency, osteoporosis primarily involves loss of bone density without abnormalities in bone mineralization. Understanding osteoporosis emphasizes the importance of bone remodeling imbalance, with heightened osteoclast activity exceeding osteoblast function, causing porous, fragile bones.
Osteomalacia: Causes and Risk Factors
Osteomalacia is characterized by the softening of bones due to defective bone mineralization, primarily caused by a deficiency in vitamin D, calcium, or phosphate. Risk factors include chronic kidney disease, malabsorption syndromes like celiac disease, certain medications such as anticonvulsants, and limited sunlight exposure. Unlike osteoporosis, which involves bone density loss, osteomalacia results from impaired bone matrix mineralization, leading to bone pain and increased fracture risk.
Osteoporosis: Causes and Risk Factors
Osteoporosis primarily involves decreased bone density and increased fracture risk due to calcium deficiency, hormonal changes, and aging, contrasting osteomalacia, which is characterized by defective bone mineralization commonly caused by vitamin D deficiency. Major risk factors for osteoporosis include advanced age, postmenopausal status, family history, low body weight, smoking, alcohol abuse, and certain medications like corticosteroids. Understanding these elements helps in distinguishing osteoporosis from osteomalacia and guides targeted prevention and treatment strategies.
Key Differences: Osteomalacia vs Osteoporosis
Osteomalacia results from defective bone mineralization due to vitamin D deficiency, leading to soft, weakened bones, whereas osteoporosis involves decreased bone density and mass caused by an imbalance between bone resorption and formation. Osteomalacia presents with bone pain and muscle weakness, whereas osteoporosis is typically asymptomatic until fractures occur. Diagnostic differentiation relies on biochemical markers such as low serum vitamin D and elevated alkaline phosphatase in osteomalacia, compared to decreased bone mineral density on DXA scans in osteoporosis.
Clinical Presentation and Symptoms Comparison
Osteomalacia presents with diffuse bone pain, muscle weakness, and difficulty walking due to defective bone mineralization, whereas osteoporosis is characterized by asymptomatic bone loss until fractures occur, particularly in the hip, spine, and wrist. Clinical examination of osteomalacia often reveals bone tenderness and proximal muscle weakness, contrasting with osteoporosis where skeletal deformities such as kyphosis and height loss may be evident after fractures. Laboratory findings in osteomalacia typically show low serum calcium and phosphate levels with elevated alkaline phosphatase, while osteoporosis displays normal biochemical markers despite reduced bone mineral density on DXA scans.
Diagnosis Methods for Osteomalacia and Osteoporosis
Diagnosis of osteomalacia primarily involves blood tests measuring serum calcium, phosphate, alkaline phosphatase, and vitamin D levels, alongside bone biopsies or radiologic imaging revealing Looser's zones or pseudofractures. Osteoporosis diagnosis frequently utilizes dual-energy X-ray absorptiometry (DEXA) scans to assess bone mineral density, which helps identify fractures risk and bone loss severity. Distinguishing between osteomalacia and osteoporosis relies on correlating biochemical markers with imaging, as osteomalacia shows mineralization defects while osteoporosis features decreased bone density without mineralization impairment.
Treatment Strategies: Osteomalacia
Treatment strategies for osteomalacia primarily focus on correcting vitamin D deficiency and calcium imbalance through supplementation of vitamin D3 or D2 and oral calcium. In cases caused by malabsorption or chronic kidney disease, addressing the underlying disorder and administering activated vitamin D analogs such as calcitriol are essential for effective bone mineralization. Regular monitoring of serum calcium, phosphate, and alkaline phosphatase levels guides therapy adjustments to ensure optimal bone health restoration.
Treatment Strategies: Osteoporosis
Treatment strategies for osteoporosis primarily include bisphosphonates such as alendronate and risedronate, which inhibit bone resorption and improve bone mineral density. Calcium and vitamin D supplementation are critical to support bone health alongside lifestyle modifications like weight-bearing exercises to enhance bone strength. In severe cases, anabolic agents such as teriparatide stimulate bone formation, offering a targeted approach distinct from treatments for osteomalacia, which focus on addressing vitamin D deficiency and calcium absorption.
Prevention, Management, and Patient Outcomes
Osteomalacia prevention centers on adequate vitamin D and calcium intake to promote proper bone mineralization, whereas osteoporosis prevention emphasizes maintaining bone density through weight-bearing exercise and pharmacologic interventions like bisphosphonates. Management of osteomalacia involves correcting underlying deficiencies with high-dose vitamin D and addressing causes such as malabsorption, while osteoporosis treatment targets reducing fracture risk via bone-strengthening medications and lifestyle modifications. Patient outcomes in osteomalacia typically improve significantly with vitamin D repletion, leading to pain relief and bone healing, whereas osteoporosis management aims to stabilize bone density and minimize fracture incidence, which can have lasting impacts on mobility and quality of life.
Osteomalacia and Osteoporosis Infographic
 libterm.com
libterm.com