Encephalitis is a serious inflammation of the brain, often caused by viral infections or autoimmune reactions, leading to symptoms such as headaches, fever, confusion, and seizures. Early diagnosis and treatment are critical to prevent long-term neurological damage and improve recovery chances. Explore the rest of this article to understand the causes, symptoms, and treatment options for encephalitis and how you can safeguard your health.
Table of Comparison
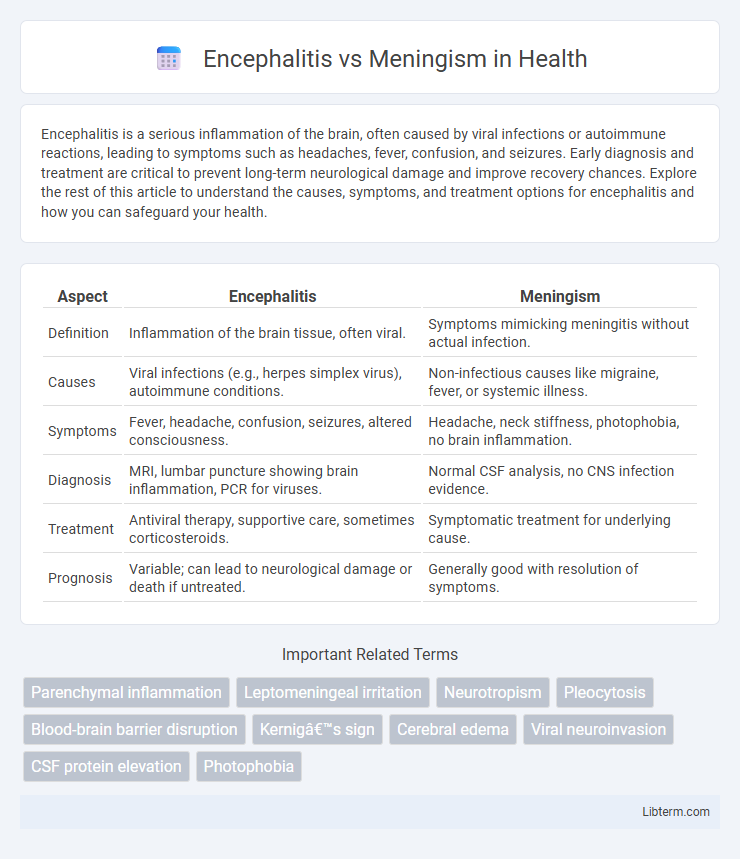
| Aspect | Encephalitis | Meningism |
|---|---|---|
| Definition | Inflammation of the brain tissue, often viral. | Symptoms mimicking meningitis without actual infection. |
| Causes | Viral infections (e.g., herpes simplex virus), autoimmune conditions. | Non-infectious causes like migraine, fever, or systemic illness. |
| Symptoms | Fever, headache, confusion, seizures, altered consciousness. | Headache, neck stiffness, photophobia, no brain inflammation. |
| Diagnosis | MRI, lumbar puncture showing brain inflammation, PCR for viruses. | Normal CSF analysis, no CNS infection evidence. |
| Treatment | Antiviral therapy, supportive care, sometimes corticosteroids. | Symptomatic treatment for underlying cause. |
| Prognosis | Variable; can lead to neurological damage or death if untreated. | Generally good with resolution of symptoms. |
Introduction to Encephalitis and Meningism
Encephalitis is an acute inflammatory condition of the brain parenchyma caused primarily by viral infections, leading to symptoms such as fever, headache, altered mental status, and neurological deficits. Meningism refers to a clinical syndrome characterized by signs of meningeal irritation, including neck stiffness, photophobia, and headache, without actual meningeal inflammation or infection. Differentiating encephalitis from meningism is crucial for targeted treatment, as encephalitis involves direct brain involvement while meningism results from meningeal irritation often secondary to systemic illness.
Definitions and Key Differences
Encephalitis is an inflammation of the brain tissue caused primarily by viral infections, resulting in neurological symptoms such as seizures, confusion, and altered consciousness. Meningism refers to a clinical syndrome characterized by symptoms of meningeal irritation like neck stiffness, photophobia, and headache, typically without actual meningitis or brain infection. The key difference lies in encephalitis involving brain parenchyma inflammation, whereas meningism indicates meningeal irritation without confirmed infectious inflammation.
Causes and Risk Factors
Encephalitis primarily results from viral infections such as herpes simplex virus or arboviruses, while meningism is usually caused by non-infectious conditions like migraine, dehydration, or fever without true meningitis. Risk factors for encephalitis include immunosuppression, age extremes, and geographic exposure to vectors like mosquitoes or ticks. Meningism often occurs in younger patients with systemic infections but lacks the serious central nervous system inflammation seen in encephalitis.
Pathophysiology of Encephalitis
Encephalitis involves inflammation of the brain parenchyma caused primarily by viral infections such as herpes simplex virus, leading to neuronal damage and brain edema. The pathophysiology includes direct viral invasion or immune-mediated injury resulting in altered blood-brain barrier permeability, microglial activation, and cytokine release. Unlike meningism, which reflects meningeal irritation without brain tissue inflammation, encephalitis affects brain function and structure, often causing neurological deficits.
Pathophysiology of Meningism
Meningism refers to the triad of headache, neck stiffness, and photophobia arising from meningeal irritation without actual inflammation or infection of the meninges, often triggered by viral illnesses or systemic inflammation. Its pathophysiology involves the irritation of sensory nerve endings in the dura mater and cerebral blood vessels, leading to reflex muscle spasm and symptoms mimicking meningitis. Unlike encephalitis, which involves direct brain parenchymal inflammation, meningism results from non-infectious meningeal irritation and does not cause neuronal injury or altered mental status.
Clinical Presentation and Symptoms
Encephalitis typically presents with altered mental status, seizures, focal neurological deficits, and fever, reflecting inflammation of the brain parenchyma. Meningism manifests with headache, neck stiffness, photophobia, and fever, symptoms indicating meningeal irritation without actual infection or inflammation of the central nervous system. Distinguishing features include the presence of neurological dysfunction in encephalitis, while meningism lacks these focal neurological signs.
Diagnostic Approaches: Encephalitis vs Meningism
Encephalitis diagnosis relies heavily on neuroimaging techniques like MRI to detect brain inflammation and lumbar puncture to analyze cerebrospinal fluid (CSF) for viral pathogens and elevated white blood cells. Meningism diagnosis primarily involves clinical assessment of meningeal irritation signs such as neck stiffness, supported by lumbar puncture findings showing normal or slightly elevated CSF without evidence of infection. Polymerase chain reaction (PCR) testing in CSF is crucial for differentiating viral encephalitis from meningism, guiding appropriate treatment strategies.
Treatment and Management Strategies
Encephalitis treatment primarily involves antiviral medications such as acyclovir for herpes simplex virus along with supportive care including seizure management and intracranial pressure monitoring, while corticosteroids may be used in certain autoimmune cases. Management of meningism focuses on addressing the underlying cause, typically bacterial or viral meningitis, with empirical intravenous antibiotics or antivirals and symptomatic relief through analgesics, hydration, and monitoring for complications like increased intracranial pressure. Both conditions require prompt hospitalization, neurological assessment, and sometimes critical care support to optimize outcomes and prevent long-term neurological deficits.
Potential Complications and Prognosis
Encephalitis often leads to severe complications such as persistent neurological deficits, seizures, and cognitive impairments, with prognosis varying based on the causative virus and timeliness of antiviral treatment. Meningism, characterized by meningeal irritation symptoms without actual meningitis, generally has a benign course with minimal risk of long-term complications or neurological damage. Early differentiation between encephalitis and meningism is crucial for preventing adverse outcomes and guiding appropriate management strategies.
Prevention and Public Health Considerations
Encephalitis prevention involves vaccination against viruses like West Nile, herpes simplex, and measles, alongside mosquito control programs to reduce vector exposure. Public health strategies emphasize early detection, isolation of infectious cases, and public education on symptom recognition to mitigate outbreaks. Meningism, a non-infectious condition mimicking meningitis symptoms, requires differential diagnosis to avoid unnecessary antibiotic use and ensure appropriate patient management.
Encephalitis Infographic
 libterm.com
libterm.com