Bactericidal agents work by killing bacteria directly, disrupting their cell walls or metabolic processes to prevent reproduction and infection. These substances are essential in treating bacterial infections and are commonly found in antibiotics, disinfectants, and antiseptics. Explore the full article to understand how bactericidal methods can protect your health effectively.
Table of Comparison
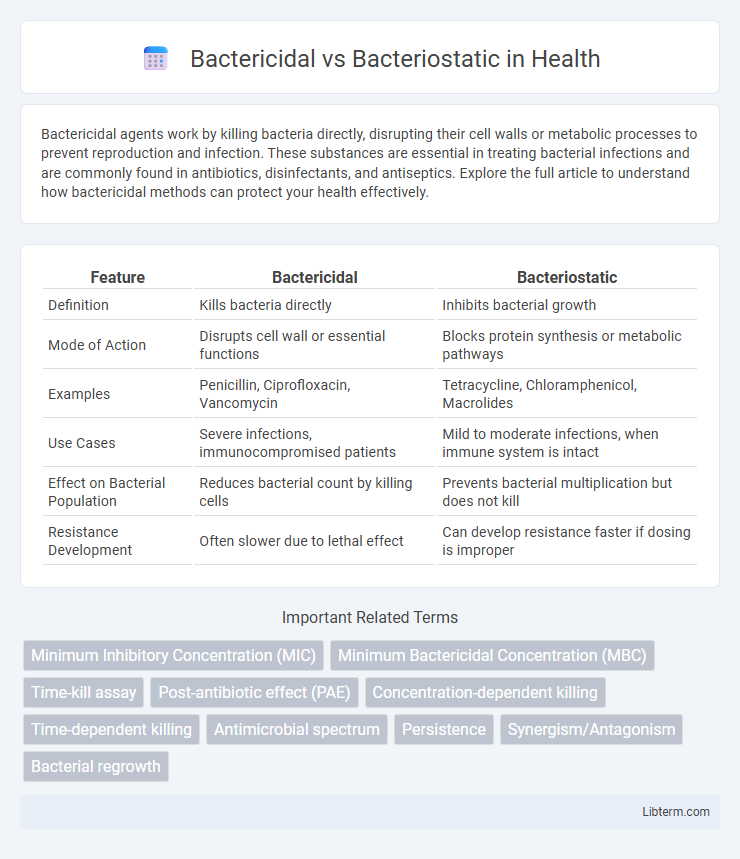
| Feature | Bactericidal | Bacteriostatic |
|---|---|---|
| Definition | Kills bacteria directly | Inhibits bacterial growth |
| Mode of Action | Disrupts cell wall or essential functions | Blocks protein synthesis or metabolic pathways |
| Examples | Penicillin, Ciprofloxacin, Vancomycin | Tetracycline, Chloramphenicol, Macrolides |
| Use Cases | Severe infections, immunocompromised patients | Mild to moderate infections, when immune system is intact |
| Effect on Bacterial Population | Reduces bacterial count by killing cells | Prevents bacterial multiplication but does not kill |
| Resistance Development | Often slower due to lethal effect | Can develop resistance faster if dosing is improper |
Introduction to Bactericidal and Bacteriostatic Agents
Bactericidal agents directly kill bacteria by disrupting essential cellular processes such as cell wall synthesis, leading to bacterial cell death. Bacteriostatic agents inhibit bacterial growth and reproduction without killing the bacteria outright, allowing the immune system to eliminate the pathogens. Understanding the mechanisms of bactericidal and bacteriostatic agents is crucial for effective antibiotic therapy and infection management.
Defining Bactericidal and Bacteriostatic
Bactericidal agents directly kill bacteria by disrupting essential cellular functions such as cell wall synthesis, leading to bacterial cell death. Bacteriostatic agents inhibit bacterial growth and reproduction without killing the bacteria, relying on the host's immune system to eliminate the infection. Understanding the mechanism of action distinguishes bactericidal antibiotics like penicillin from bacteriostatic drugs like tetracycline.
Mechanisms of Action
Bactericidal agents kill bacteria by disrupting critical cellular functions such as cell wall synthesis, protein synthesis, or DNA replication, leading to bacterial cell death. Bacteriostatic agents inhibit bacterial growth and reproduction by interfering with protein synthesis or metabolic pathways, effectively halting bacterial proliferation without directly killing the cells. Understanding these distinct mechanisms aids in selecting appropriate antimicrobial therapies based on infection severity and patient immune status.
Examples of Bactericidal Antibiotics
Examples of bactericidal antibiotics include penicillins, cephalosporins, aminoglycosides, and fluoroquinolones, which kill bacteria by disrupting cell wall synthesis or interfering with DNA replication. Vancomycin targets gram-positive bacteria by inhibiting cell wall formation, while aminoglycosides like gentamicin bind to the 30S ribosomal subunit, causing mistranslation and bacterial cell death. Fluoroquinolones such as ciprofloxacin inhibit bacterial DNA gyrase and topoisomerase IV, leading to lethal DNA damage in pathogens.
Examples of Bacteriostatic Antibiotics
Bacteriostatic antibiotics inhibit bacterial growth and reproduction without directly killing the bacteria, allowing the immune system to eliminate the infection. Common examples of bacteriostatic antibiotics include tetracyclines, such as doxycycline, macrolides like erythromycin and azithromycin, and sulfonamides such as sulfamethoxazole. These agents target bacterial protein synthesis or metabolic pathways, effectively halting bacterial proliferation.
Clinical Applications and Considerations
Bactericidal agents eliminate bacteria directly, making them crucial in treating severe infections such as endocarditis, meningitis, and sepsis where rapid bacterial eradication is essential. Bacteriostatic drugs inhibit bacterial growth and rely on the host immune system to clear the infection, proving effective in less critical infections or when minimizing bacterial resistance is prioritized. Clinicians must consider infection severity, immune status, and tissue penetration when selecting between bactericidal and bacteriostatic antibiotics to optimize therapeutic outcomes.
Factors Influencing Antibiotic Selection
Antibiotic selection depends on factors such as the infection site, pathogen type, and patient's immune status, where bactericidal agents are preferred for severe infections like endocarditis or meningitis due to their ability to kill bacteria directly. Bacteriostatic antibiotics inhibit bacterial growth, relying on the immune system to clear the infection, making them suitable for less severe or uncomplicated infections. Other considerations include drug toxicity, pharmacokinetics, resistance patterns, and patient allergies, all influencing whether a bactericidal or bacteriostatic antibiotic is optimal for treatment.
Resistance Development: Bactericidal vs Bacteriostatic
Bactericidal agents actively kill bacteria, reducing the risk of resistance development by eliminating pathogens more effectively, whereas bacteriostatic agents inhibit bacterial growth, allowing the immune system to clear the infection but potentially facilitating resistance if the bacteria survive prolonged exposure. Resistance development is often slower with bactericidal antibiotics due to their lethal action, while bacteriostatic drugs may select for resistant strains as bacteria adapt to inhibited, yet viable, conditions. Understanding these dynamics is crucial for selecting appropriate antimicrobial therapy to minimize resistance emergence in clinical settings.
Laboratory Testing and Interpretation
Laboratory testing differentiates bactericidal from bacteriostatic agents by assessing microbial viability through minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) assays, where bactericidal agents typically exhibit an MBC close to the MIC, indicating effective killing of bacteria. Interpretation of these results guides clinical decisions; bactericidal agents are preferred for severe infections or immunocompromised patients, whereas bacteriostatic agents inhibit bacterial growth, allowing the immune system to eliminate pathogens. Accurate differentiation ensures appropriate antibiotic selection, optimizing treatment outcomes and minimizing resistance development.
Summary: Choosing the Right Antibacterial Approach
Bactericidal agents kill bacteria directly, making them essential for treating severe infections like endocarditis or meningitis, where rapid bacterial elimination is critical. Bacteriostatic agents inhibit bacterial growth, allowing the immune system to clear the infection, often preferred in less severe cases or when minimizing resistance development is a priority. Selecting between bactericidal and bacteriostatic treatments depends on infection severity, patient immune status, and the specific bacterial pathogen involved.
Bactericidal Infographic
 libterm.com
libterm.com