Bathmotropic effects refer to changes in the excitability of cardiac muscle cells, influencing how easily the heart responds to stimuli. Positive bathmotropic agents increase the heart's responsiveness, potentially altering rhythm, while negative agents decrease excitability, stabilizing cardiac activity. Discover how understanding bathmotropic properties can impact your heart health by exploring the rest of this article.
Table of Comparison
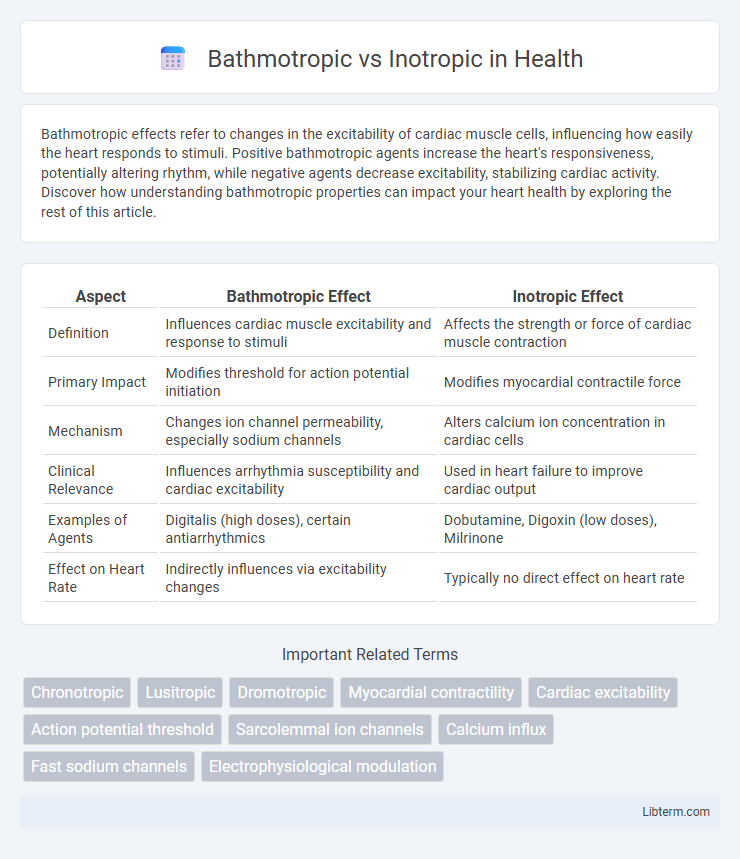
| Aspect | Bathmotropic Effect | Inotropic Effect |
|---|---|---|
| Definition | Influences cardiac muscle excitability and response to stimuli | Affects the strength or force of cardiac muscle contraction |
| Primary Impact | Modifies threshold for action potential initiation | Modifies myocardial contractile force |
| Mechanism | Changes ion channel permeability, especially sodium channels | Alters calcium ion concentration in cardiac cells |
| Clinical Relevance | Influences arrhythmia susceptibility and cardiac excitability | Used in heart failure to improve cardiac output |
| Examples of Agents | Digitalis (high doses), certain antiarrhythmics | Dobutamine, Digoxin (low doses), Milrinone |
| Effect on Heart Rate | Indirectly influences via excitability changes | Typically no direct effect on heart rate |
Introduction to Cardiac Muscle Properties
Bathmotropic and inotropic effects describe different properties of cardiac muscle function; bathmotropy refers to the excitability of cardiac cells, influencing their threshold for activation, while inotropy relates to the strength of myocardial contraction. Bathmotropic changes alter the responsiveness of cardiac muscle fibers to stimulation, impacting the initiation of action potentials. Inotropic modulation affects contractile force by modifying calcium availability and interaction within cardiac myocytes, critical for maintaining effective cardiac output.
Defining Bathmotropy and Inotropy
Bathmotropy refers to the excitability of cardiac muscle cells, specifically their responsiveness to stimuli that initiate action potentials. Inotropy describes the force or strength of myocardial contraction, directly influencing the heart's ability to pump blood effectively. Both bathmotropic and inotropic properties are crucial for maintaining optimal cardiac function and are key targets in cardiovascular pharmacology.
Mechanisms of Bathmotropic Effects
Bathmotropic effects refer to changes in the excitability of cardiac muscle fibers, primarily influenced by alterations in the threshold potential required to trigger action potentials. This mechanism involves modulation of ion channel activity, especially sodium and potassium channels, which affects the ease of depolarization in myocardial cells. Unlike inotropic effects that modify the force of contraction, bathmotropic effects govern the responsiveness of cardiac tissue to electrical stimuli, impacting arrhythmogenesis and conduction velocity.
Mechanisms of Inotropic Effects
Inotropic effects primarily influence the force of cardiac muscle contraction by modulating the intracellular calcium concentration within cardiomyocytes. Positive inotropic agents increase calcium influx through L-type calcium channels and enhance calcium release from the sarcoplasmic reticulum, thereby strengthening myocardial contractility. Negative inotropic effects result from decreased calcium availability or interference with calcium binding to troponin, reducing the heart's contractile force.
Key Differences Between Bathmotropic and Inotropic Actions
Bathmotropic effects refer to changes in the excitability of cardiac muscle fibers, influencing the threshold for action potential generation, whereas inotropic effects modify the force of cardiac muscle contraction by affecting myocardial contractility. Bathmotropic alterations primarily impact the conduction system's responsiveness to stimuli, while inotropic actions directly affect the strength and efficiency of heartbeats through calcium ion regulation within cardiomyocytes. These distinct mechanisms underlie the therapeutic approaches targeting arrhythmias with bathmotropic agents and heart failure with inotropic drugs.
Physiological Significance in Cardiac Function
Bathmotropic effects influence the excitability of cardiac muscle cells by altering the threshold for action potential generation, which is crucial for regulating heart rhythm and preventing arrhythmias. Inotropic effects modify the force of cardiac muscle contraction by affecting intracellular calcium levels, directly impacting cardiac output and myocardial performance. Together, bathmotropic and inotropic properties coordinate to maintain optimal cardiac function under varying physiological conditions.
Clinical Implications of Bathmotropic Modulation
Bathmotropic effects involve changes in cardiac excitability, impacting the threshold for action potential initiation without altering contraction strength, crucial in managing arrhythmias and excitability disorders. Clinical modulation of bathmotropy can help stabilize abnormal cardiac rhythms by adjusting the ease of myocardial cell depolarization, often targeted in antiarrhythmic therapies. Understanding bathmotropic influences guides precise pharmacological interventions to prevent tachyarrhythmias and enhance patient outcomes in cardiac electrophysiology.
Therapeutic Uses of Inotropic Agents
Inotropic agents primarily enhance myocardial contractility, playing a critical role in managing heart failure and cardiogenic shock. These drugs, such as digoxin and dobutamine, increase cardiac output by improving the strength of heart muscle contractions without significantly altering heart rate. Bathmotropic effects, which influence the excitability of cardiac muscle, are less directly targeted in therapy but can impact arrhythmogenesis during inotropic treatment.
Common Drugs Affecting Bathmotropy and Inotropy
Common drugs affecting bathmotropy primarily include lidocaine and quinidine, which modulate the excitability of cardiac cells by altering sodium channel activity, thus influencing the threshold potential. Inotropic agents such as digoxin, dobutamine, and milrinone enhance myocardial contractility by increasing intracellular calcium concentrations or sensitizing contractile proteins, critically improving cardiac output in heart failure patients. Beta-adrenergic agonists and calcium channel blockers also significantly impact both bathmotropic and inotropic properties by regulating calcium influx and adrenergic stimulation in cardiac tissue.
Summary and Future Perspectives
Bathmotropic effects alter cardiac excitability by modifying the threshold for action potential initiation, while inotropic effects influence myocardial contractility by changing the force of contraction. Understanding the molecular mechanisms and ion channel targets responsible for these effects offers promising avenues for developing pharmacological agents to treat arrhythmias and heart failure. Future research is expected to focus on selective modulators that precisely regulate bathmotropic and inotropic responses without adverse side effects, enhancing patient-specific cardiac therapy.
Bathmotropic Infographic
 libterm.com
libterm.com