Corneal ulcers are open sores on the cornea caused by infections, dry eyes, or trauma and can lead to severe pain, redness, and vision impairment. Immediate diagnosis and treatment with antibiotics or antifungal medications are crucial to prevent complications like scarring or vision loss. Discover more about symptoms, causes, and effective treatments to protect your eye health in the detailed article ahead.
Table of Comparison
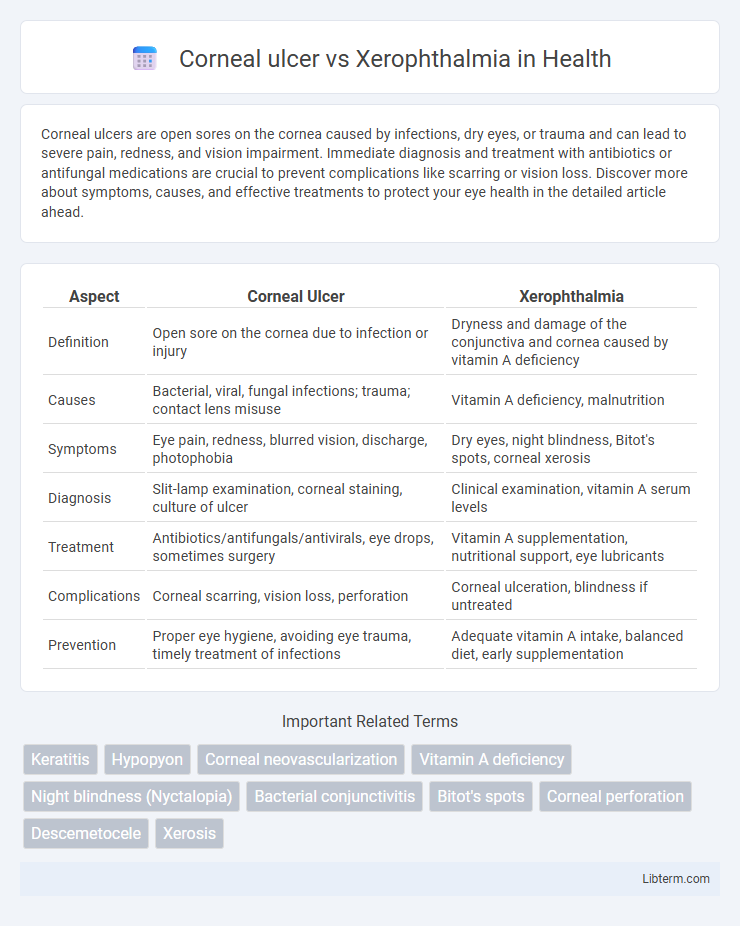
| Aspect | Corneal Ulcer | Xerophthalmia |
|---|---|---|
| Definition | Open sore on the cornea due to infection or injury | Dryness and damage of the conjunctiva and cornea caused by vitamin A deficiency |
| Causes | Bacterial, viral, fungal infections; trauma; contact lens misuse | Vitamin A deficiency, malnutrition |
| Symptoms | Eye pain, redness, blurred vision, discharge, photophobia | Dry eyes, night blindness, Bitot's spots, corneal xerosis |
| Diagnosis | Slit-lamp examination, corneal staining, culture of ulcer | Clinical examination, vitamin A serum levels |
| Treatment | Antibiotics/antifungals/antivirals, eye drops, sometimes surgery | Vitamin A supplementation, nutritional support, eye lubricants |
| Complications | Corneal scarring, vision loss, perforation | Corneal ulceration, blindness if untreated |
| Prevention | Proper eye hygiene, avoiding eye trauma, timely treatment of infections | Adequate vitamin A intake, balanced diet, early supplementation |
Introduction to Corneal Ulcer and Xerophthalmia
Corneal ulcer is an open sore on the cornea caused by infections, trauma, or underlying eye conditions leading to pain, redness, and potential vision loss. Xerophthalmia is a severe dryness of the conjunctiva and cornea due to vitamin A deficiency, resulting in night blindness and keratinization of the ocular surface. Both conditions affect corneal health but differ in etiology, with corneal ulcers typically linked to microbial invasion and xerophthalmia to nutritional deficiencies.
Definition and Key Differences
Corneal ulcer is an open sore on the cornea caused by infections, trauma, or dry eye, leading to pain, redness, and vision impairment. Xerophthalmia is a condition marked by severe dryness of the conjunctiva and cornea due to vitamin A deficiency, resulting in night blindness and potential corneal damage. The key difference lies in corneal ulcer being primarily an infectious or injury-related lesion, whereas xerophthalmia stems from nutritional deficiency affecting eye moisture and surface integrity.
Etiology and Risk Factors
Corneal ulcer primarily results from bacterial, viral, fungal, or parasitic infections, often associated with trauma, contact lens misuse, or dry eye conditions that compromise corneal integrity. Xerophthalmia stems from vitamin A deficiency, commonly caused by malnutrition, malabsorption disorders, or chronic alcoholism, leading to impaired tear production and conjunctival metaplasia. Risk factors for corneal ulcer include ocular surface disease, immunosuppression, and exposure to contaminated water, while xerophthalmia is linked to poverty, insufficient dietary intake, and systemic illnesses affecting vitamin A metabolism.
Clinical Presentation and Symptoms
Corneal ulcer presents as a painful, red eye with decreased vision, photophobia, and a visible white or grayish spot on the cornea, often accompanied by tearing and discharge. Xerophthalmia manifests primarily with dryness, night blindness, Bitot's spots, and conjunctival dryness due to vitamin A deficiency, leading to a rough, keratinized surface of the conjunctiva and cornea. While corneal ulcers exhibit acute inflammation and ulceration, xerophthalmia reflects chronic keratinization and epithelial damage, emphasizing distinct clinical features in diagnosis.
Pathophysiology of Corneal Ulcer
Corneal ulcer primarily results from an infection caused by bacteria, fungi, viruses, or parasites that penetrate the corneal epithelium, leading to inflammation, stromal degradation, and necrosis. This breakdown of the corneal tissue disrupts the protective barrier, allowing immune cells to infiltrate and release enzymes that degrade the stroma further. Xerophthalmia, in contrast, is caused by vitamin A deficiency leading to dryness and keratinization of the conjunctiva and cornea but does not involve corneal stromal infection or ulceration as seen in corneal ulcers.
Pathophysiology of Xerophthalmia
Xerophthalmia results from chronic vitamin A deficiency leading to decreased tear production and keratinization of the conjunctival and corneal epithelium. This causes dryness, loss of goblet cells, and impaired mucous layer, disrupting the ocular surface homeostasis. Unlike corneal ulcers, which involve localized epithelial breakdown due to infection or injury, xerophthalmia involves a progressive degeneration of the ocular surface linked to systemic nutritional deficiency.
Diagnostic Approaches
Corneal ulcer diagnosis relies heavily on slit-lamp examination and fluorescein staining to detect epithelial defects and assess the depth of corneal involvement. Xerophthalmia diagnosis involves clinical evaluation of conjunctival dryness, Bitot's spots, and serum retinol levels to determine vitamin A deficiency. Imaging modalities are less prominent in xerophthalmia but essential in corneal ulcer to monitor healing and complications.
Treatment and Management Strategies
Corneal ulcer treatment prioritizes immediate antimicrobial therapy using antibiotics, antifungals, or antivirals based on the infection cause, accompanied by pain management and sometimes corticosteroids to reduce inflammation after initial control. Xerophthalmia management centers on vitamin A supplementation to address deficiency, along with lubricating eye drops and managing underlying causes like malnutrition to prevent corneal damage. Regular monitoring and supportive care play crucial roles in both conditions to prevent complications and preserve vision.
Prognosis and Complications
Corneal ulcer prognosis varies by cause and treatment timeliness, with bacterial ulcers having a higher risk of vision loss and scarring complications, while fungal ulcers often require prolonged therapy. Xerophthalmia, primarily caused by vitamin A deficiency, can lead to keratomalacia and irreversible blindness if untreated, but early intervention can improve prognosis. Complications of corneal ulcers include perforation and endophthalmitis, whereas xerophthalmia complications involve night blindness and systemic immune impairment.
Prevention and Patient Education
Corneal ulcer prevention emphasizes prompt treatment of eye infections, maintaining proper hygiene, and avoiding contact lens misuse to reduce microbial invasion. Xerophthalmia prevention centers on ensuring adequate vitamin A intake through diet or supplements, especially in populations at risk of deficiency, to maintain tear production and ocular surface health. Patient education should highlight the importance of early symptom recognition and adherence to preventive measures tailored to each condition's etiology.
Corneal ulcer Infographic
 libterm.com
libterm.com