Pancytopenia is a medical condition characterized by the reduction of all three blood cell types: red blood cells, white blood cells, and platelets, leading to symptoms like fatigue, infections, and bleeding. Understanding the causes, such as bone marrow disorders, infections, or autoimmune diseases, is crucial for effective diagnosis and treatment. Explore the full article to learn more about your options for managing and addressing pancytopenia.
Table of Comparison
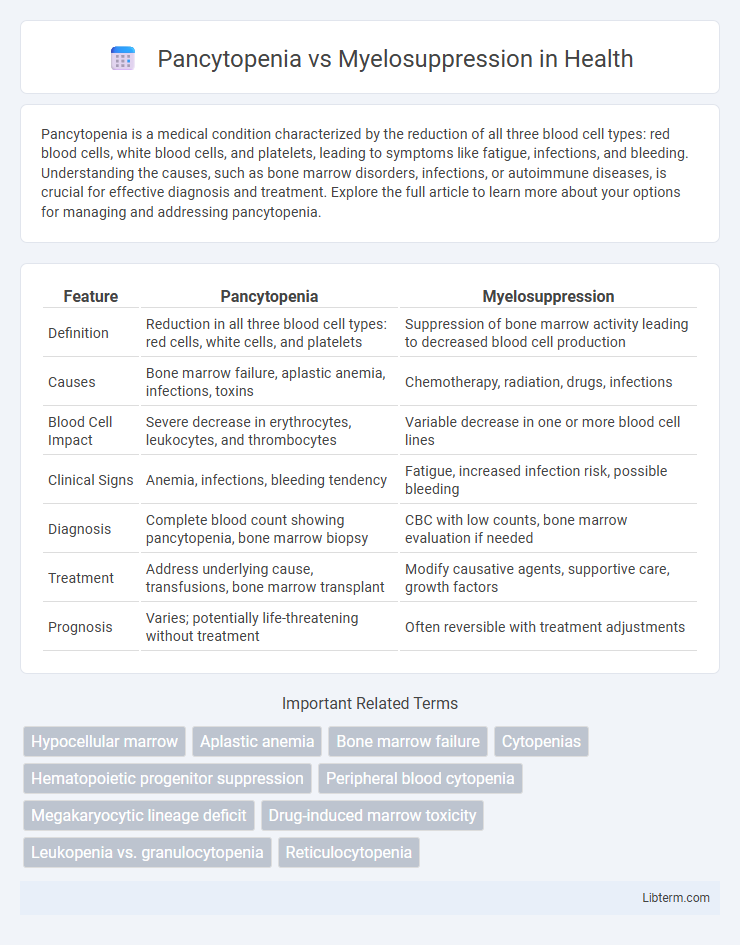
| Feature | Pancytopenia | Myelosuppression |
|---|---|---|
| Definition | Reduction in all three blood cell types: red cells, white cells, and platelets | Suppression of bone marrow activity leading to decreased blood cell production |
| Causes | Bone marrow failure, aplastic anemia, infections, toxins | Chemotherapy, radiation, drugs, infections |
| Blood Cell Impact | Severe decrease in erythrocytes, leukocytes, and thrombocytes | Variable decrease in one or more blood cell lines |
| Clinical Signs | Anemia, infections, bleeding tendency | Fatigue, increased infection risk, possible bleeding |
| Diagnosis | Complete blood count showing pancytopenia, bone marrow biopsy | CBC with low counts, bone marrow evaluation if needed |
| Treatment | Address underlying cause, transfusions, bone marrow transplant | Modify causative agents, supportive care, growth factors |
| Prognosis | Varies; potentially life-threatening without treatment | Often reversible with treatment adjustments |
Introduction to Pancytopenia and Myelosuppression
Pancytopenia is a clinical condition characterized by the reduction of all three blood cell lines: red blood cells, white blood cells, and platelets, often resulting from bone marrow failure or destruction. Myelosuppression refers specifically to the decreased bone marrow activity, leading to suppressed production of blood cells, commonly caused by chemotherapy, radiation, or certain medications. Understanding the distinction is critical for diagnosis and treatment, as pancytopenia describes the hematologic outcome while myelosuppression defines the underlying pathophysiological process.
Defining Pancytopenia: Key Features
Pancytopenia is characterized by a significant reduction in all three blood cell types: red blood cells, white blood cells, and platelets, indicating a broad bone marrow failure. It is often a clinical manifestation resulting from diverse conditions such as aplastic anemia, leukemia, or severe infections. Unlike myelosuppression, which primarily denotes bone marrow suppression typically induced by chemotherapy or radiation, pancytopenia reflects a more generalized deficiency affecting multiple cell lineages, resulting in symptoms like anemia, increased infection risk, and bleeding tendencies.
Understanding Myelosuppression: Core Aspects
Myelosuppression is a condition characterized by the decreased production of blood cells due to bone marrow suppression, often resulting from chemotherapy, radiation, or certain drugs. It primarily leads to pancytopenia, which is a significant reduction in red cells, white cells, and platelets, causing increased risk of anemia, infection, and bleeding. Effective management of myelosuppression involves monitoring blood counts, identifying the underlying cause, and supportive therapies like growth factors or transfusions to restore hematopoietic function.
Etiology: Causes of Pancytopenia vs Myelosuppression
Pancytopenia typically results from bone marrow failure caused by conditions such as aplastic anemia, hematologic malignancies like leukemia, and severe vitamin deficiencies, whereas myelosuppression is primarily induced by external factors including chemotherapy, radiation therapy, and certain drugs that directly inhibit bone marrow activity. Infectious agents like parvovirus B19 and HIV can contribute to both pancytopenia and myelosuppression by disrupting hematopoiesis. Autoimmune diseases and toxic exposures also play significant roles in the etiology of pancytopenia and myelosuppression, emphasizing their overlapping but distinct causative mechanisms.
Pathophysiological Differences
Pancytopenia is characterized by a simultaneous reduction in red blood cells, white blood cells, and platelets due to bone marrow failure or infiltration, resulting in impaired hematopoiesis across multiple lineages. Myelosuppression specifically refers to the decreased production of blood cells caused by toxic effects on bone marrow progenitor cells, commonly induced by chemotherapy or radiation therapy, which transiently suppresses hematopoietic activity. The primary pathophysiological difference lies in pancytopenia being a broader clinical manifestation of marrow insufficiency or destruction, while myelosuppression denotes a reversible, treatment-related suppression of marrow function affecting one or more cell lines.
Clinical Manifestations and Symptoms
Pancytopenia presents with simultaneous anemia, leukopenia, and thrombocytopenia, leading to symptoms such as fatigue, pallor, increased susceptibility to infections, and bleeding tendencies including petechiae and purpura. Myelosuppression primarily causes a reduction in bone marrow activity, manifesting as decreased production of one or more blood cell lines, which results in symptoms reflecting the specific cytopenia, such as leukopenia-induced infections or thrombocytopenia-related bleeding. Clinical evaluation often reveals overlapping signs but pancytopenia involves a global reduction in all blood cell types, whereas myelosuppression may affect selective lineages depending on the underlying cause or treatment.
Diagnostic Approaches and Laboratory Findings
Pancytopenia is characterized by a reduction in red blood cells, white blood cells, and platelets, often requiring a complete blood count (CBC) and bone marrow biopsy to assess marrow cellularity and identify underlying causes such as aplastic anemia or leukemia. Myelosuppression primarily results from chemotherapy or radiation therapy, leading to decreased production of blood cells, diagnosed through serial CBC monitoring and evaluating the extent of marrow suppression without necessarily showing marrow infiltration or fibrosis. Bone marrow aspiration and cytogenetic analysis are critical in differentiating pancytopenia due to marrow failure from transient myelosuppression, guiding appropriate treatment strategies.
Common Underlying Diseases and Risk Factors
Pancytopenia often results from bone marrow failure syndromes such as aplastic anemia, leukemia, and myelodysplastic syndromes, while myelosuppression commonly arises from chemotherapy, radiation therapy, and certain infections like HIV or tuberculosis. Risk factors for pancytopenia include autoimmune disorders, exposure to toxins, and congenital bone marrow defects, whereas myelosuppression is primarily linked to cytotoxic drug exposure and viral infections disrupting hematopoiesis. Both conditions share common disease associations like malignancies and infections but differ significantly in etiology and clinical management due to their distinct pathophysiological mechanisms.
Treatment Strategies: Pancytopenia vs Myelosuppression
Treatment strategies for pancytopenia focus on addressing the underlying cause, such as bone marrow failure, infections, or autoimmune diseases. Myelosuppression management often involves dose adjustment or discontinuation of causative agents like chemotherapy, along with supportive measures like growth factors and transfusions. Both conditions require careful monitoring of blood counts and supportive care to prevent complications like infections and bleeding.
Prognosis, Complications, and Patient Outcomes
Pancytopenia, characterized by a deficiency of all three blood cell types, often results from bone marrow failure or peripheral destruction, and its prognosis depends on the underlying cause and severity, with complications including severe infections, bleeding, and anemia-related symptoms. Myelosuppression, typically induced by chemotherapy or radiation, leads to a temporary reduction in bone marrow activity, with outcomes largely favoring recovery upon treatment cessation but with risks of infections, hemorrhage, and delayed healing during the suppression period. Patient outcomes for pancytopenia vary widely, from full recovery to chronic illness or mortality, while myelosuppression generally has a predictable course with appropriate supportive care and monitoring.
Pancytopenia Infographic
 libterm.com
libterm.com