Primary biliary cholangitis is a chronic autoimmune liver disease characterized by the gradual destruction of bile ducts, leading to bile buildup and liver damage. Early diagnosis and management are essential to slow disease progression and improve quality of life. Discover more about symptoms, treatment options, and lifestyle tips in the rest of the article.
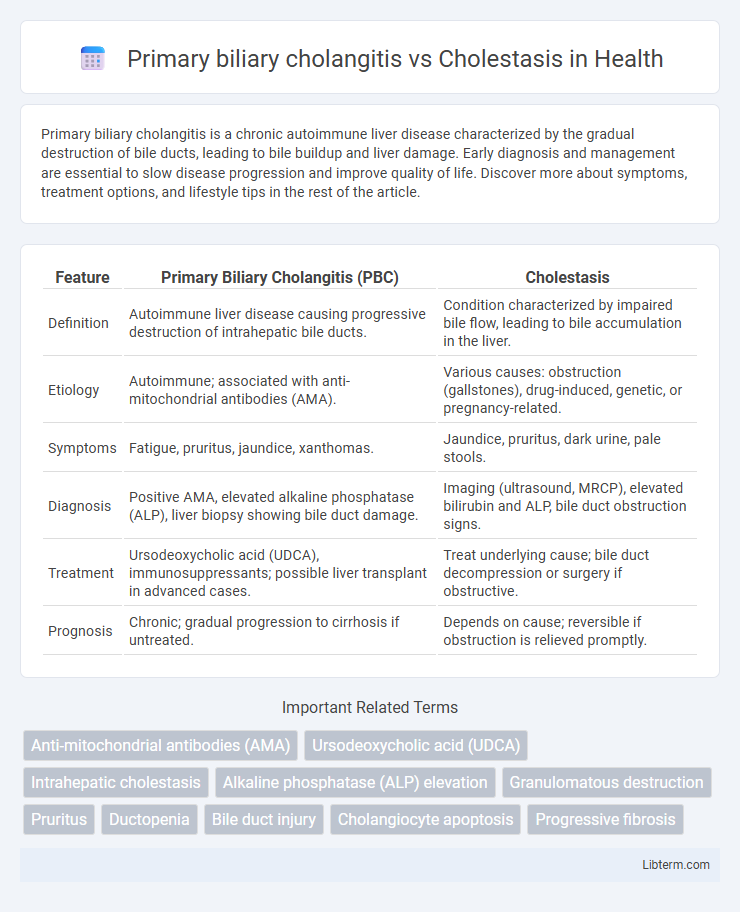
Table of Comparison
| Feature | Primary Biliary Cholangitis (PBC) | Cholestasis |
|---|---|---|
| Definition | Autoimmune liver disease causing progressive destruction of intrahepatic bile ducts. | Condition characterized by impaired bile flow, leading to bile accumulation in the liver. |
| Etiology | Autoimmune; associated with anti-mitochondrial antibodies (AMA). | Various causes: obstruction (gallstones), drug-induced, genetic, or pregnancy-related. |
| Symptoms | Fatigue, pruritus, jaundice, xanthomas. | Jaundice, pruritus, dark urine, pale stools. |
| Diagnosis | Positive AMA, elevated alkaline phosphatase (ALP), liver biopsy showing bile duct damage. | Imaging (ultrasound, MRCP), elevated bilirubin and ALP, bile duct obstruction signs. |
| Treatment | Ursodeoxycholic acid (UDCA), immunosuppressants; possible liver transplant in advanced cases. | Treat underlying cause; bile duct decompression or surgery if obstructive. |
| Prognosis | Chronic; gradual progression to cirrhosis if untreated. | Depends on cause; reversible if obstruction is relieved promptly. |
Introduction to Primary Biliary Cholangitis and Cholestasis
Primary Biliary Cholangitis (PBC) is a chronic autoimmune liver disease characterized by progressive destruction of intrahepatic bile ducts leading to cholestasis and eventual liver fibrosis. Cholestasis refers to the impairment of bile flow causing accumulation of bile acids in the liver, which can be intrahepatic or extrahepatic in origin and result from various conditions including PBC. Understanding the pathophysiological differences is critical for diagnosis and management, as PBC specifically involves immune-mediated bile duct injury while cholestasis encompasses a broader spectrum of bile flow obstruction.
Definition and Overview of Primary Biliary Cholangitis
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease characterized by progressive destruction of intrahepatic bile ducts, leading to cholestasis and potential cirrhosis. PBC primarily affects middle-aged women and is marked by antimitochondrial antibodies (AMA) presence and elevated alkaline phosphatase levels. Cholestasis refers broadly to impaired bile flow from liver to duodenum caused by various conditions, including PBC, bile duct obstruction, or drug-induced liver injury.
Definition and Types of Cholestasis
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease characterized by the gradual destruction of intrahepatic bile ducts, leading to cholestasis and progressive liver fibrosis. Cholestasis refers to the impairment of bile flow, which can be classified into intrahepatic cholestasis, resulting from hepatocellular or bile duct dysfunction, and extrahepatic cholestasis caused by obstruction of large bile ducts outside the liver. Understanding these distinctions is crucial for diagnosing and managing conditions like PBC, which represents a specific form of intrahepatic cholestasis.
Causes and Risk Factors
Primary biliary cholangitis (PBC) is an autoimmune disease characterized by the destruction of intrahepatic bile ducts, primarily affecting middle-aged women and associated with genetic predisposition and environmental triggers such as infections or chemical exposure. Cholestasis results from impaired bile flow due to either intrahepatic causes like drugs, infections, or genetic disorders, or extrahepatic causes such as bile duct obstruction by gallstones or tumors. Risk factors for PBC include a family history of autoimmune diseases and the presence of antimitochondrial antibodies, while cholestasis risk factors vary widely depending on the underlying etiology, including medication use and obstructive lesions.
Pathophysiology: How the Diseases Develop
Primary biliary cholangitis (PBC) is an autoimmune liver disease characterized by progressive destruction of intrahepatic bile ducts, leading to cholestasis and fibrosis. Cholestasis results from impaired bile flow due to obstruction, hepatocellular dysfunction, or genetic defects affecting bile secretion. In PBC, immune-mediated damage targets mitochondrial antigens within biliary epithelial cells, while cholestasis involves disrupted bile acid transport and accumulation causing hepatocellular injury.
Clinical Presentation and Symptoms
Primary biliary cholangitis (PBC) typically presents with fatigue, pruritus, and jaundice, often accompanied by hepatomegaly and xanthomas in chronic cases. Cholestasis manifests through impaired bile flow, leading to symptoms such as intense itching, dark urine, pale stools, and jaundice due to elevated serum bilirubin levels. Both conditions involve cholestatic liver enzyme patterns, but PBC is an autoimmune disorder with specific antimitochondrial antibodies, whereas cholestasis can be caused by intrahepatic or extrahepatic obstruction.
Diagnostic Approaches and Laboratory Findings
Primary biliary cholangitis (PBC) is diagnosed through elevated antimitochondrial antibodies (AMA) in over 90% of cases, alongside increased alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) levels, reflecting chronic autoimmune destruction of intrahepatic bile ducts. Cholestasis presents with elevated bilirubin, ALP, and GGT but lacks specific autoantibodies, often requiring imaging studies such as ultrasound or MRCP to identify obstructive causes or intrahepatic bile duct injury. Liver biopsy may differentiate PBC's distinctive nonsuppurative destructive cholangitis and granulomas from cholestasis patterns, aiding precise diagnosis and management.
Treatment Strategies and Management
Primary biliary cholangitis (PBC) treatment primarily involves ursodeoxycholic acid (UDCA) to slow disease progression, with obeticholic acid as a second-line therapy for UDCA non-responders, alongside symptom management for pruritus and fatigue. Cholestasis management depends on its etiology, requiring removal or treatment of the underlying cause such as gallstones, bile duct obstruction, or drug-induced cholestasis, along with supportive care including bile acid sequestrants and symptom relief. Both conditions may require monitoring liver function and potential liver transplantation in advanced cases where medical therapy is insufficient.
Prognosis and Complications
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease characterized by progressive destruction of intrahepatic bile ducts leading to fibrosis and potentially cirrhosis, with complications including portal hypertension, osteoporosis, and increased risk of hepatocellular carcinoma; prognosis has improved with ursodeoxycholic acid therapy, but advanced stages require liver transplantation. Cholestasis, a condition marked by impaired bile flow, can be intrahepatic or extrahepatic with causes ranging from drug-induced injury to bile duct obstruction; complications include fat-soluble vitamin deficiencies, pruritus, and progression to biliary cirrhosis if unresolved, with prognosis depending on the underlying etiology and response to treatment. Early diagnosis and targeted management optimize outcomes in both conditions, reducing the risk of liver failure and associated morbidity.
Key Differences Between Primary Biliary Cholangitis and Cholestasis
Primary biliary cholangitis (PBC) is a chronic autoimmune liver disease characterized by the destruction of intrahepatic bile ducts, leading to progressive cholestasis and fibrosis, while cholestasis broadly refers to the impairment or blockage of bile flow from the liver to the duodenum caused by various conditions. PBC specifically involves the presence of antimitochondrial antibodies (AMAs) and predominantly affects middle-aged women, contrasting with cholestasis, which can result from mechanical obstruction, drug-induced injury, or systemic diseases and does not necessarily present with autoimmune markers. Diagnosis of PBC relies on elevated alkaline phosphatase (ALP), positive AMA, and liver biopsy showing nonsuppurative destructive cholangitis, whereas cholestasis diagnosis depends on imaging to identify bile duct obstruction and biochemical markers indicating impaired bile secretion.
Primary biliary cholangitis Infographic
 libterm.com
libterm.com