A renal abscess is a localized collection of pus within or around the kidney, typically caused by a bacterial infection that can lead to severe pain, fever, and urinary symptoms. Early diagnosis and targeted treatment, often involving antibiotics or drainage, are crucial to prevent complications such as sepsis or kidney damage. Discover more about the symptoms, causes, and effective treatments to protect Your kidney health in the rest of this article.
Table of Comparison
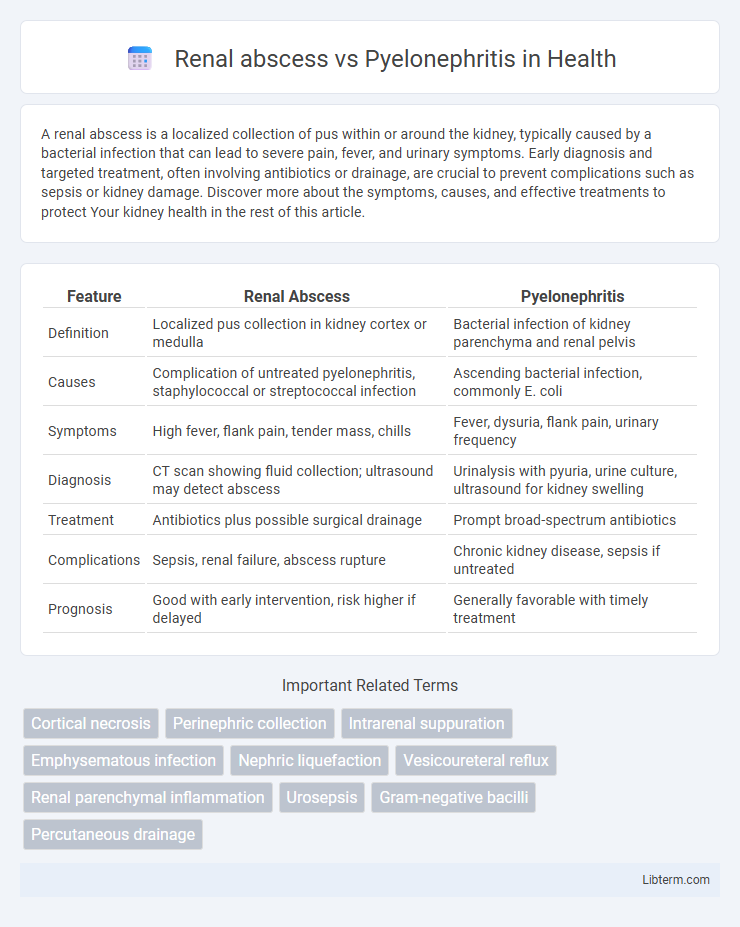
| Feature | Renal Abscess | Pyelonephritis |
|---|---|---|
| Definition | Localized pus collection in kidney cortex or medulla | Bacterial infection of kidney parenchyma and renal pelvis |
| Causes | Complication of untreated pyelonephritis, staphylococcal or streptococcal infection | Ascending bacterial infection, commonly E. coli |
| Symptoms | High fever, flank pain, tender mass, chills | Fever, dysuria, flank pain, urinary frequency |
| Diagnosis | CT scan showing fluid collection; ultrasound may detect abscess | Urinalysis with pyuria, urine culture, ultrasound for kidney swelling |
| Treatment | Antibiotics plus possible surgical drainage | Prompt broad-spectrum antibiotics |
| Complications | Sepsis, renal failure, abscess rupture | Chronic kidney disease, sepsis if untreated |
| Prognosis | Good with early intervention, risk higher if delayed | Generally favorable with timely treatment |
Introduction to Renal Abscess and Pyelonephritis
Renal abscess is a localized collection of pus within the kidney tissues often resulting from bacterial infection or secondary to untreated pyelonephritis. Pyelonephritis represents an acute or chronic bacterial infection of the renal pelvis and kidney parenchyma frequently caused by ascending urinary tract infections. Differentiating between renal abscess and pyelonephritis relies on imaging studies, clinical presentation, and laboratory findings as both conditions share overlapping symptoms such as fever, flank pain, and urinary disturbances.
Epidemiology and Risk Factors
Renal abscesses, less common than pyelonephritis, occur primarily in patients with diabetes mellitus, urinary tract obstructions, or immunosuppression, affecting approximately 1 in 10,000 hospital admissions. Pyelonephritis is a more prevalent urinary tract infection, especially among sexually active women, pregnant women, and patients with vesicoureteral reflux or urinary catheterization; its incidence ranges from 15 to 17 cases per 10,000 outpatient visits. Both conditions share risk factors such as diabetes and urinary tract abnormalities but differ significantly in their clinical severity and potential for systemic complications.
Pathogenesis and Etiology
Renal abscesses result from localized bacterial infection leading to pus-filled cavities within the renal parenchyma, often caused by Staphylococcus aureus or ascending urinary tract infections with Escherichia coli. Pyelonephritis involves acute inflammation of the renal pelvis and interstitium, primarily due to ascending bacterial infection, most commonly by Escherichia coli, Proteus, and Klebsiella species. Both conditions arise from bacterial invasion but differ in lesion localization and severity of infection, with renal abscesses representing a contained, severe suppurative complication of pyelonephritis or systemic bacteremia.
Clinical Presentation and Symptoms
Renal abscess typically presents with localized flank pain, high-grade fever, and prolonged malaise, often accompanied by a palpable tender mass on examination. Pyelonephritis manifests with sudden onset of fever, chills, dysuria, and costovertebral angle tenderness, frequently associated with urinary symptoms such as frequency and urgency. Both conditions share systemic signs like fever and malaise but differ in severity and duration, with renal abscess often showing persistent symptoms despite antibiotic therapy.
Diagnostic Criteria and Imaging Modalities
Renal abscess is characterized by a localized collection of pus within the kidney, diagnosed through imaging modalities such as contrast-enhanced CT, which reveals a well-defined hypodense lesion with rim enhancement, whereas pyelonephritis presents as a diffuse infection of the renal parenchyma detected by ultrasound showing enlarged, hypoechoic areas or CT demonstrating striated nephrogram and renal enlargement. Diagnostic criteria for renal abscess include persistent fever despite antibiotic therapy, flank pain, and leukocytosis, with imaging confirming the presence of an encapsulated fluid collection, while pyelonephritis diagnosis relies on clinical symptoms such as dysuria, fever, costovertebral angle tenderness, urinalysis showing pyuria, and imaging to rule out complications. MRI serves as an alternative imaging tool for both conditions, offering high sensitivity in detecting inflammatory changes and abscess cavities without radiation exposure.
Laboratory Findings and Differentiation
Renal abscess typically presents with elevated white blood cell count, increased erythrocyte sedimentation rate (ESR), and positive blood or urine cultures indicating localized infection, whereas pyelonephritis shows similar laboratory abnormalities but often with more diffuse urinary tract infection markers. Urinalysis in pyelonephritis reveals pyuria, bacteriuria, and sometimes hematuria, while renal abscess may have sterile urinalysis if abscess is isolated and not communicating with the collecting system. Imaging such as contrast-enhanced CT scan is crucial for differentiation, showing a well-defined fluid collection in renal abscess, contrasting with diffuse renal enlargement and striated nephrogram typical of pyelonephritis.
Treatment Approaches and Management Strategies
Renal abscess treatment primarily involves prolonged intravenous antibiotics targeting causative organisms such as Staphylococcus aureus and Gram-negative bacilli, often coupled with percutaneous drainage or surgical intervention for abscesses larger than 3 cm. Pyelonephritis management relies on empirical broad-spectrum antibiotics like fluoroquinolones or third-generation cephalosporins, with hospitalization and intravenous therapy reserved for severe or complicated cases, including those with systemic symptoms or impaired renal function. Early identification of the condition through imaging techniques, such as ultrasound or CT scan, guides appropriate treatment choices to prevent progression and complications.
Complications and Prognosis
Renal abscesses often lead to severe complications such as sepsis, renal cortical destruction, and chronic kidney disease if not promptly drained, while pyelonephritis may progress to renal scarring and recurrent urinary tract infections. The prognosis of renal abscesses typically requires surgical or percutaneous drainage combined with antibiotics, with delayed treatment increasing morbidity and mortality risks. Pyelonephritis generally has a favorable prognosis with appropriate antibiotic therapy, but complicated or untreated cases can result in long-term renal impairment and systemic infection.
Prevention and Risk Reduction
Effective prevention of renal abscess and pyelonephritis centers on managing underlying urinary tract infections (UTIs) promptly with appropriate antibiotics to prevent bacterial spread. Risk reduction involves maintaining good personal hygiene, adequate hydration, and controlling chronic conditions such as diabetes mellitus that predispose to infection. Regular medical follow-up and early treatment of any urinary symptoms are crucial to avoiding complications like renal abscess formation.
Key Differences: Renal Abscess vs Pyelonephritis
Renal abscess is a localized collection of pus within the kidney parenchyma, often resulting from untreated or severe pyelonephritis, characterized by focal pain, fluctuance on imaging, and possible systemic toxicity. Pyelonephritis is an acute bacterial infection of the renal pelvis and kidney tissue, presenting with fever, flank pain, and dysuria but generally lacking a distinct abscess cavity on ultrasound or CT scans. Treatment for renal abscesses typically requires prolonged antibiotic therapy combined with percutaneous drainage, whereas pyelonephritis is managed primarily with antibiotics alone.
Renal abscess Infographic
 libterm.com
libterm.com