Valve replacement is a critical procedure to restore proper heart function when one or more valves are damaged or diseased. The surgery involves removing the faulty valve and implanting a mechanical or biological substitute to ensure efficient blood flow. Discover more about the types, risks, and recovery process to understand how valve replacement can impact your heart health.
Table of Comparison
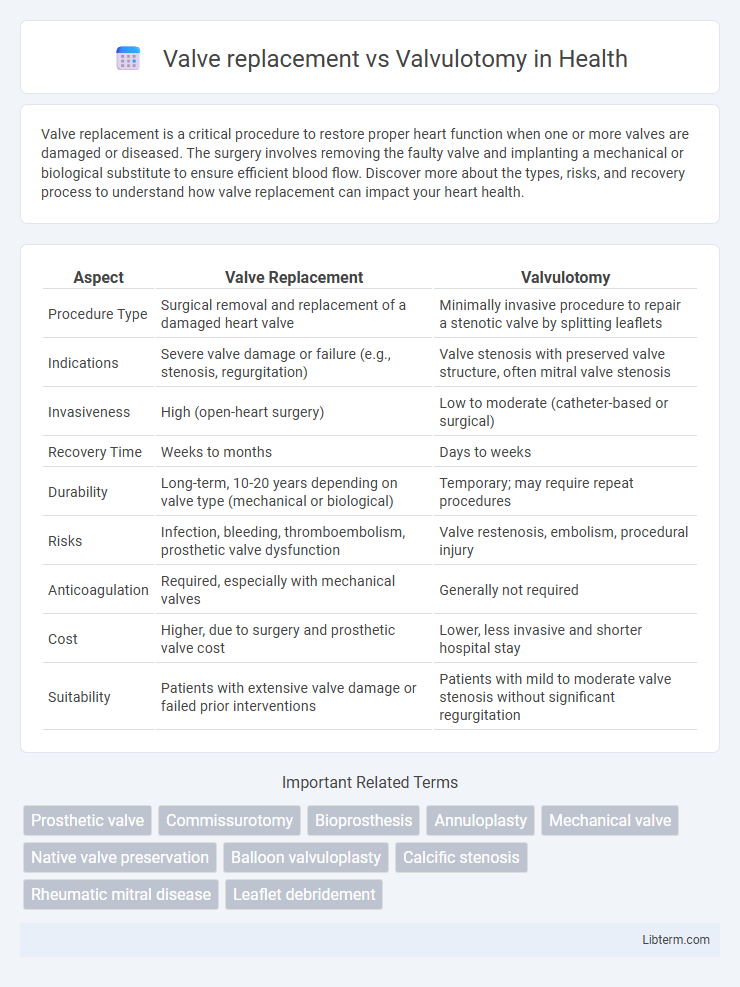
| Aspect | Valve Replacement | Valvulotomy |
|---|---|---|
| Procedure Type | Surgical removal and replacement of a damaged heart valve | Minimally invasive procedure to repair a stenotic valve by splitting leaflets |
| Indications | Severe valve damage or failure (e.g., stenosis, regurgitation) | Valve stenosis with preserved valve structure, often mitral valve stenosis |
| Invasiveness | High (open-heart surgery) | Low to moderate (catheter-based or surgical) |
| Recovery Time | Weeks to months | Days to weeks |
| Durability | Long-term, 10-20 years depending on valve type (mechanical or biological) | Temporary; may require repeat procedures |
| Risks | Infection, bleeding, thromboembolism, prosthetic valve dysfunction | Valve restenosis, embolism, procedural injury |
| Anticoagulation | Required, especially with mechanical valves | Generally not required |
| Cost | Higher, due to surgery and prosthetic valve cost | Lower, less invasive and shorter hospital stay |
| Suitability | Patients with extensive valve damage or failed prior interventions | Patients with mild to moderate valve stenosis without significant regurgitation |
Overview of Valve Replacement and Valvulotomy
Valve replacement involves surgically removing a damaged heart valve and implanting a mechanical or biological prosthetic valve to restore normal blood flow. Valvulotomy, also known as valvuloplasty, is a less invasive procedure that repairs a stenotic valve by widening its opening through balloon dilation or surgical incision. Both procedures aim to improve valve function, with valve replacement typically indicated for severely damaged valves and valvulotomy preferred for less advanced stenosis.
Indications for Valve Replacement
Valve replacement is primarily indicated in cases of severe valve stenosis or regurgitation causing significant symptoms or left ventricular dysfunction, especially when valve repair or valvulotomy is not feasible. It is favored for patients with irreversible valve damage, calcification, or infected valves in endocarditis. Valve replacement provides durable hemodynamic improvement and symptom relief when valvulotomy cannot adequately restore valve function.
Indications for Valvulotomy
Valvulotomy is primarily indicated for patients with rheumatic mitral stenosis who exhibit thickened, fused valve leaflets and subvalvular apparatus without significant calcification, allowing improved leaflet mobility. It is preferred in cases where valve preservation is possible and right heart function must be maintained, especially in young patients or those contraindicated for valve replacement. Valve replacement is generally reserved for severe, calcified, or regurgitant lesions unsuitable for repair through valvulotomy.
Surgical Techniques: Valve Replacement
Valve replacement involves excising the damaged valve and implanting a mechanical or bioprosthetic valve to restore normal blood flow. This surgical technique requires precise suturing and positioning to ensure valve competency and minimize paravalvular leakage. Advances in valve replacement include minimally invasive approaches and transcatheter valve implantation, reducing operative risk and recovery time.
Surgical Techniques: Valvulotomy
Valvulotomy involves the strategic incision or dilation of a stenotic valve to restore adequate blood flow while preserving the native valve structure, often utilizing balloon catheter techniques or direct surgical cutting. This procedure minimizes the need for prosthetic valve implantation, reducing risks associated with valve replacement such as thrombosis, structural valve deterioration, and the requirement for lifelong anticoagulation therapy. Valvulotomy is preferred in suitable patients with valve stenosis where retaining native valve function offers better long-term hemodynamic outcomes and fewer complications compared to valve replacement.
Risks and Complications of Each Procedure
Valve replacement carries risks including infection, blood clots, valve malfunction, and complications from anticoagulation therapy. Valvulotomy involves potential complications such as valve restenosis, embolism, and damage to the valve or surrounding heart tissue. Both procedures require careful monitoring for heart rhythm abnormalities and may necessitate repeat interventions depending on patient-specific factors.
Recovery and Rehabilitation Differences
Recovery after valve replacement typically involves a longer hospital stay and more intensive rehabilitation compared to valvulotomy due to the invasiveness of the procedure and the need for anticoagulation management. Valvulotomy patients often experience shorter recovery times with less postoperative pain and quicker return to normal activities, as the procedure preserves native valve structures. Rehabilitation protocols for valve replacement emphasize cardiac rehabilitation, wound care, and monitoring for prosthetic valve complications, while valvulotomy focuses on improving valve function and managing symptoms with minimal intervention.
Long-Term Outcomes and Prognosis
Valve replacement offers a more definitive long-term solution for severe valvular heart disease by restoring optimal valve function and reducing mortality rates compared to valvulotomy, which may have higher rates of restenosis and recurrent symptoms. Long-term studies demonstrate that valve replacement patients experience improved survival and lower rates of re-intervention over a 10- to 20-year follow-up period, particularly in cases of aortic and mitral valve pathology. While valvulotomy can provide symptomatic relief, its prognosis is limited by progressive valve degeneration, resulting in less favorable outcomes compared to valve replacement in terms of durability and quality of life.
Patient Selection Criteria
Patient selection criteria for valve replacement primarily include patients with severe valve dysfunction, significant structural damage, or when repair is unlikely to restore adequate valve function, especially in cases of calcific aortic stenosis or rheumatic heart disease. Valvulotomy is typically indicated for patients with less extensive valve pathology, such as commissural fusion without significant leaflet destruction, often in younger patients or those with rheumatic mitral stenosis to preserve native valve structure. The decision hinges on echocardiographic findings, valve anatomy, patient age, comorbidities, and the likelihood of long-term valve function restoration.
Emerging Trends in Valve Repair and Replacement
Emerging trends in valve repair and replacement emphasize minimally invasive techniques and bioprosthetic valve advancements to improve patient outcomes and longevity. Transcatheter valve replacement (TAVR) and valve-in-valve procedures are gaining popularity for high-risk patients, reducing recovery time and procedural risks. Research into tissue-engineered valves and robotic-assisted valvulotomy offers promising directions for enhancing durability and precision in valve repair strategies.
Valve replacement Infographic
 libterm.com
libterm.com