Cirrhosis is a chronic liver condition characterized by irreversible scarring that impairs liver function and can lead to severe complications such as liver failure and portal hypertension. Early diagnosis and lifestyle changes, including avoiding alcohol and managing underlying causes, are crucial to slowing disease progression and maintaining your overall health. Learn more about cirrhosis symptoms, treatments, and prevention strategies by reading the rest of this article.
Table of Comparison
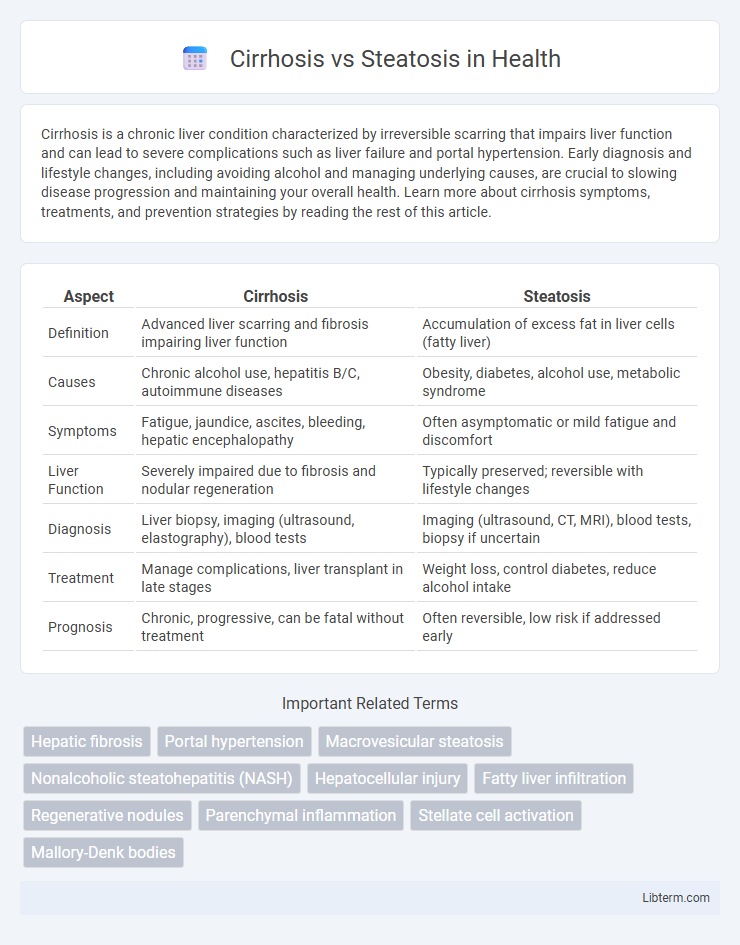
| Aspect | Cirrhosis | Steatosis |
|---|---|---|
| Definition | Advanced liver scarring and fibrosis impairing liver function | Accumulation of excess fat in liver cells (fatty liver) |
| Causes | Chronic alcohol use, hepatitis B/C, autoimmune diseases | Obesity, diabetes, alcohol use, metabolic syndrome |
| Symptoms | Fatigue, jaundice, ascites, bleeding, hepatic encephalopathy | Often asymptomatic or mild fatigue and discomfort |
| Liver Function | Severely impaired due to fibrosis and nodular regeneration | Typically preserved; reversible with lifestyle changes |
| Diagnosis | Liver biopsy, imaging (ultrasound, elastography), blood tests | Imaging (ultrasound, CT, MRI), blood tests, biopsy if uncertain |
| Treatment | Manage complications, liver transplant in late stages | Weight loss, control diabetes, reduce alcohol intake |
| Prognosis | Chronic, progressive, can be fatal without treatment | Often reversible, low risk if addressed early |
Introduction to Cirrhosis and Steatosis
Cirrhosis is a chronic liver disease characterized by irreversible scarring and impaired liver function caused by long-term damage such as hepatitis or alcohol abuse. Steatosis, also known as fatty liver disease, involves the accumulation of fat in liver cells and is often reversible with lifestyle changes. Both conditions impact liver health but differ significantly in severity and progression, with cirrhosis representing advanced liver damage.
Defining Cirrhosis: Causes and Mechanisms
Cirrhosis is a chronic liver disease characterized by irreversible scarring and impaired liver function caused primarily by long-term liver damage from hepatitis, alcohol abuse, or fatty liver disease. It arises when continuous liver injury triggers excessive collagen deposition and fibrosis, disrupting normal liver architecture and blood flow. Unlike steatosis, which is the accumulation of fat in liver cells often reversible and less severe, cirrhosis represents advanced liver damage with significant clinical consequences.
Understanding Steatosis: Causes and Risk Factors
Steatosis, commonly known as fatty liver disease, is characterized by the accumulation of fat in liver cells, primarily caused by excessive alcohol consumption, obesity, and insulin resistance linked to type 2 diabetes. Non-alcoholic fatty liver disease (NAFLD) is a prevalent manifestation of steatosis, often associated with metabolic syndrome factors such as hypertension, dyslipidemia, and central adiposity. Early identification of risk factors like high-fat diets and sedentary lifestyles is critical for managing steatosis and preventing progression to more severe liver conditions such as cirrhosis.
Key Differences Between Cirrhosis and Steatosis
Cirrhosis is characterized by extensive liver scarring and impaired liver function, often resulting from chronic liver diseases such as hepatitis or long-term alcohol abuse, whereas steatosis refers to the accumulation of fat within liver cells, commonly known as fatty liver. Cirrhosis involves irreversible damage with symptoms including jaundice, portal hypertension, and liver failure, while steatosis is usually reversible and may be asymptomatic or cause mild liver inflammation. The prognosis and treatment strategies differ significantly, with cirrhosis requiring management of complications and possible liver transplantation, whereas steatosis focuses on lifestyle changes to reduce liver fat and prevent progression.
Signs and Symptoms: How Cirrhosis and Steatosis Present
Cirrhosis typically presents with symptoms such as jaundice, ascites, fatigue, muscle wasting, and spider angiomas, reflecting advanced liver damage and impaired function. Steatosis, or fatty liver disease, often remains asymptomatic but may cause mild fatigue, discomfort in the upper right abdomen, and hepatomegaly. Elevated liver enzymes are common in both conditions, but cirrhosis symptoms indicate chronic liver scarring, whereas steatosis signals fat accumulation without significant fibrosis.
Diagnostic Approaches for Cirrhosis vs Steatosis
Diagnostic approaches for cirrhosis primarily include liver biopsy, elastography (FibroScan), and imaging studies such as ultrasound, CT, or MRI to assess fibrosis extent and liver architecture changes. Steatosis diagnosis relies heavily on imaging techniques like ultrasound with controlled attenuation parameter (CAP), MRI-PDFF (proton density fat fraction), and occasionally liver biopsy to quantify fat accumulation and exclude inflammation or fibrosis. Serum biomarkers and liver function tests complement imaging findings in differentiating cirrhosis from simple steatosis by evaluating liver damage severity and fibrosis presence.
Progression: From Steatosis to Cirrhosis
Steatosis, characterized by the accumulation of fat in liver cells, can progress to cirrhosis when persistent liver injury triggers inflammation and fibrosis. Chronic hepatic steatosis leads to nonalcoholic steatohepatitis (NASH), which accelerates extracellular matrix deposition and disrupts liver architecture. This fibrotic progression ultimately results in cirrhosis, marked by irreversible scarring and compromised liver function.
Treatment Strategies: Cirrhosis vs Steatosis
Treatment strategies for cirrhosis primarily focus on managing complications, slowing disease progression, and addressing underlying causes such as viral hepatitis or alcohol use, often requiring medications like diuretics, beta-blockers, or liver transplantation in advanced stages. Steatosis, or fatty liver disease, is treated mainly through lifestyle interventions including weight loss, dietary changes, increased physical activity, and control of metabolic risk factors such as diabetes and hyperlipidemia, with pharmacologic treatments being less clearly defined. While cirrhosis treatment emphasizes preventing liver failure and managing portal hypertension, steatosis management aims to reverse fat accumulation and prevent progression to steatohepatitis and fibrosis.
Prevention and Lifestyle Modifications
Preventing cirrhosis and steatosis primarily involves managing risk factors such as alcohol consumption, obesity, and metabolic syndrome. Adopting a balanced diet rich in fruits, vegetables, and whole grains, alongside regular physical activity, supports liver health and reduces fat accumulation. Avoiding hepatotoxic substances and controlling underlying conditions like diabetes and hypertension are critical lifestyle modifications that can halt disease progression.
Prognosis and Long-Term Outcomes
Cirrhosis is characterized by irreversible liver scarring leading to impaired liver function, significantly increasing the risk of liver failure, hepatocellular carcinoma, and mortality with a generally poor prognosis without liver transplantation. Steatosis, or fatty liver disease, often represents an early, reversible stage of liver damage with a favorable prognosis if underlying causes like obesity, alcohol use, or metabolic syndrome are addressed. Long-term outcomes for steatosis can improve substantially through lifestyle modifications, whereas cirrhosis requires ongoing medical management and surveillance to prevent complications and progression.
Cirrhosis Infographic
 libterm.com
libterm.com