Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, causing difficulty in breathing, wheezing, and coughing. Managing asthma effectively requires understanding triggers, using prescribed medications, and following a tailored action plan. Explore this article to learn how you can control asthma symptoms and improve your quality of life.
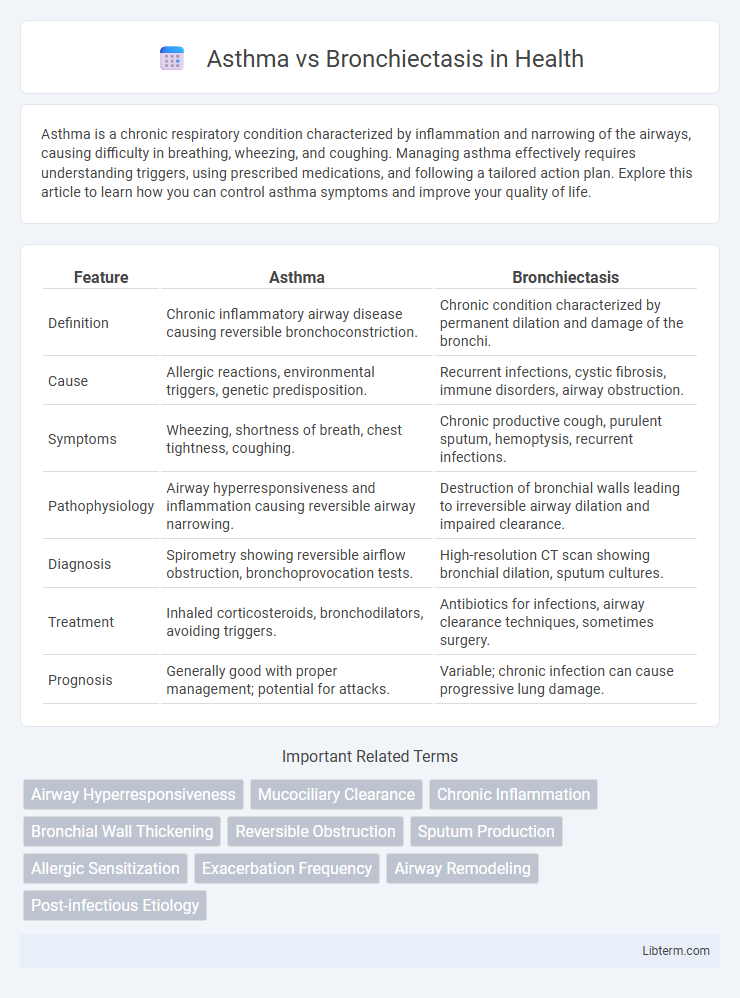
Table of Comparison
| Feature | Asthma | Bronchiectasis |
|---|---|---|
| Definition | Chronic inflammatory airway disease causing reversible bronchoconstriction. | Chronic condition characterized by permanent dilation and damage of the bronchi. |
| Cause | Allergic reactions, environmental triggers, genetic predisposition. | Recurrent infections, cystic fibrosis, immune disorders, airway obstruction. |
| Symptoms | Wheezing, shortness of breath, chest tightness, coughing. | Chronic productive cough, purulent sputum, hemoptysis, recurrent infections. |
| Pathophysiology | Airway hyperresponsiveness and inflammation causing reversible airway narrowing. | Destruction of bronchial walls leading to irreversible airway dilation and impaired clearance. |
| Diagnosis | Spirometry showing reversible airflow obstruction, bronchoprovocation tests. | High-resolution CT scan showing bronchial dilation, sputum cultures. |
| Treatment | Inhaled corticosteroids, bronchodilators, avoiding triggers. | Antibiotics for infections, airway clearance techniques, sometimes surgery. |
| Prognosis | Generally good with proper management; potential for attacks. | Variable; chronic infection can cause progressive lung damage. |
Introduction to Asthma and Bronchiectasis
Asthma is a chronic inflammatory disease of the airways characterized by reversible bronchoconstriction, airway hyperresponsiveness, and episodic airflow obstruction, often triggered by allergens or irritants. Bronchiectasis involves permanent dilation and destruction of the bronchial walls due to chronic infection or inflammation, leading to persistent cough, sputum production, and recurrent respiratory infections. Understanding the distinct pathophysiology of asthma and bronchiectasis is crucial for accurate diagnosis and targeted treatment.
Definition and Overview
Asthma is a chronic inflammatory disease of the airways characterized by reversible airflow obstruction and bronchial hyperresponsiveness, leading to symptoms such as wheezing, coughing, and shortness of breath. Bronchiectasis is a chronic lung condition marked by permanent dilation and destruction of the bronchial walls, causing persistent cough, sputum production, and recurrent respiratory infections. Both conditions affect the respiratory system but differ in pathophysiology, with asthma primarily involving airway inflammation and bronchospasm, while bronchiectasis involves structural airway damage and impaired mucus clearance.
Causes and Risk Factors
Asthma is primarily caused by inflammation and narrowing of the airways triggered by allergens, respiratory infections, or environmental factors such as pollution and tobacco smoke. Bronchiectasis results from chronic infections or conditions that damage the bronchial walls, including cystic fibrosis, immune system disorders, or severe pneumonia. Risk factors for asthma include a family history of allergic diseases, exposure to airborne irritants, and viral respiratory infections in early childhood, while bronchiectasis risk increases with repeated lung infections, impaired mucus clearance, and underlying pulmonary diseases.
Key Symptoms and Clinical Presentation
Asthma primarily presents with episodic wheezing, shortness of breath, chest tightness, and coughing, especially at night or early morning, often triggered by allergens or exercise. Bronchiectasis is characterized by chronic productive cough with large amounts of purulent sputum, recurrent respiratory infections, and sometimes hemoptysis, reflecting permanent dilation and damage of the bronchi. Both conditions can cause airflow obstruction, but asthma symptoms tend to be variable and reversible, whereas bronchiectasis involves persistent airway damage and frequent exacerbations.
Diagnostic Differences
Asthma diagnosis primarily relies on spirometry showing reversible airway obstruction and bronchial hyperresponsiveness, often confirmed with a methacholine challenge test. Bronchiectasis diagnosis involves high-resolution computed tomography (HRCT) scans revealing permanent bronchial dilation and structural lung changes, alongside sputum culture to identify chronic infections. Differentiating these conditions requires evaluating clinical history, imaging findings, and pulmonary function tests to distinguish airway inflammation from irreversible bronchial damage.
Pathophysiology: Asthma vs Bronchiectasis
Asthma is characterized by reversible airway inflammation, bronchoconstriction, and hyperresponsiveness caused by immune-mediated airway inflammation involving eosinophils and mast cells. Bronchiectasis involves irreversible dilation and destruction of the bronchial walls due to chronic infection and inflammation, leading to impaired mucociliary clearance and persistent bacterial colonization. The distinct pathophysiological mechanisms result in asthma demonstrating reversible airflow obstruction, while bronchiectasis causes permanent airway damage and progressive lung function decline.
Treatment Approaches and Management
Asthma treatment primarily involves inhaled corticosteroids and bronchodilators to reduce airway inflammation and relieve symptoms, with emphasis on trigger avoidance and long-term control medications. Bronchiectasis management includes airway clearance techniques, antibiotics for infection control, and sometimes bronchodilators, targeting sputum reduction and preventing exacerbations. Both conditions require regular monitoring, pulmonary rehabilitation, and personalized action plans to optimize respiratory function and quality of life.
Complications and Prognosis
Asthma complications primarily include persistent airway inflammation, increased risk of severe exacerbations, and potential development of airway remodeling leading to chronic obstruction. Bronchiectasis complications often involve recurrent infections, progressive lung damage, and respiratory failure due to irreversible bronchial dilatation. Prognosis for asthma generally improves with effective management, while bronchiectasis prognosis depends on infection control and underlying cause, often requiring long-term therapy to prevent decline in lung function.
Prevention Strategies
Effective prevention strategies for asthma center on reducing exposure to allergens, tobacco smoke, and air pollution to minimize airway inflammation and hyperresponsiveness. Bronchiectasis prevention emphasizes early treatment of respiratory infections, vaccination against influenza and pneumococcus, and avoiding environmental irritants to prevent chronic airway damage and dilation. Both conditions benefit from maintaining good respiratory hygiene and managing underlying health factors to reduce exacerbations and improve long-term lung function.
When to Seek Medical Attention
Seek medical attention for asthma when experiencing severe shortness of breath, chest tightness, persistent coughing, or wheezing that does not improve with use of a prescribed inhaler. Bronchiectasis requires prompt medical evaluation if symptoms include chronic productive cough with large amounts of sputum, recurrent respiratory infections, or unexplained weight loss. Early intervention in both asthma and bronchiectasis prevents complications such as respiratory failure and reduces hospitalizations.
Asthma Infographic
 libterm.com
libterm.com