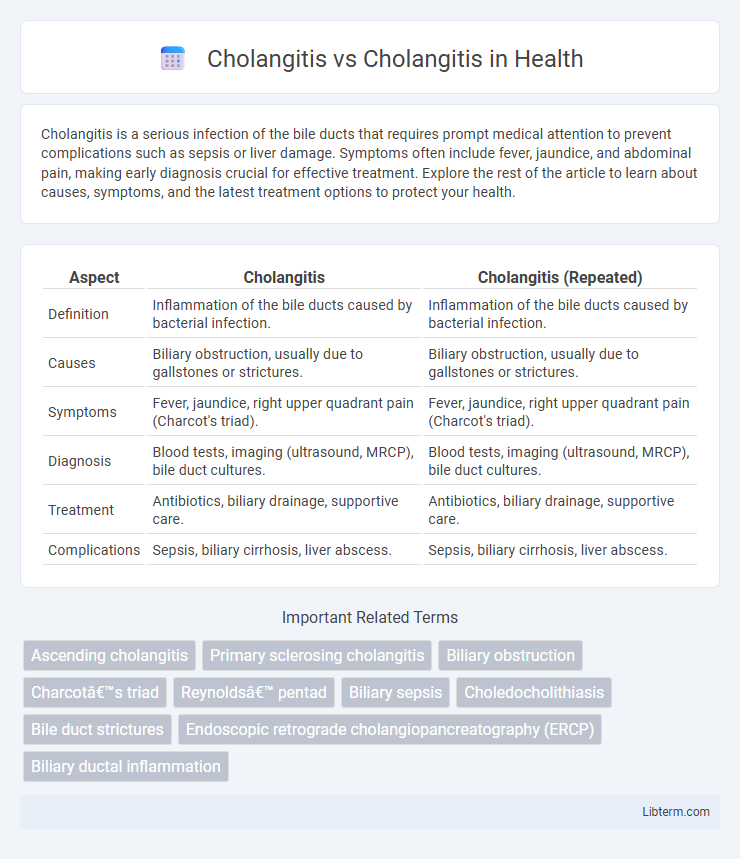
Cholangitis is a serious infection of the bile ducts that requires prompt medical attention to prevent complications such as sepsis or liver damage. Symptoms often include fever, jaundice, and abdominal pain, making early diagnosis crucial for effective treatment. Explore the rest of the article to learn about causes, symptoms, and the latest treatment options to protect your health.
Table of Comparison
| Aspect | Cholangitis | Cholangitis (Repeated) |
|---|---|---|
| Definition | Inflammation of the bile ducts caused by bacterial infection. | Inflammation of the bile ducts caused by bacterial infection. |
| Causes | Biliary obstruction, usually due to gallstones or strictures. | Biliary obstruction, usually due to gallstones or strictures. |
| Symptoms | Fever, jaundice, right upper quadrant pain (Charcot's triad). | Fever, jaundice, right upper quadrant pain (Charcot's triad). |
| Diagnosis | Blood tests, imaging (ultrasound, MRCP), bile duct cultures. | Blood tests, imaging (ultrasound, MRCP), bile duct cultures. |
| Treatment | Antibiotics, biliary drainage, supportive care. | Antibiotics, biliary drainage, supportive care. |
| Complications | Sepsis, biliary cirrhosis, liver abscess. | Sepsis, biliary cirrhosis, liver abscess. |
Introduction to Cholangitis
Cholangitis is an infection of the bile ducts typically caused by bacterial invasion due to bile duct obstruction, most often from gallstones or strictures. The condition presents with symptoms such as jaundice, fever, and right upper quadrant abdominal pain, collectively known as Charcot's triad. Early diagnosis and treatment, including antibiotics and biliary decompression, are critical to prevent severe complications like sepsis and liver damage.
Types of Cholangitis
Cholangitis primarily includes ascending cholangitis and primary sclerosing cholangitis, with ascending cholangitis caused by bacterial infection due to bile duct obstruction, presenting acute symptoms such as fever, jaundice, and abdominal pain. Primary sclerosing cholangitis is a chronic, progressive autoimmune disease characterized by inflammation and fibrosis of intrahepatic and extrahepatic bile ducts, leading to stricture formation and bile flow impairment. Distinguishing between these types is critical for diagnosis and treatment, as ascending cholangitis requires urgent antibiotic therapy and drainage, while primary sclerosing cholangitis involves long-term management and monitoring for complications like cholangiocarcinoma.
Etiology and Risk Factors
Cholangitis primarily arises from bacterial infection due to bile duct obstruction, often caused by gallstones, strictures, or tumors obstructing bile flow. Risk factors include advanced age, biliary tract instrumentation, immunosuppression, and conditions such as primary sclerosing cholangitis or malignancy of the bile ducts or pancreas. Distinguishing between acute cholangitis, characterized by infection and inflammation, and chronic cholangitis, typically linked to long-term autoimmune or progressive bile duct diseases, is essential for targeted treatment.
Clinical Presentation and Symptoms
Cholangitis presents with Charcot's triad, including right upper quadrant pain, fever, and jaundice, reflecting biliary tract infection and inflammation. In contrast, primary sclerosing cholangitis often manifests with fatigue, pruritus, and intermittent jaundice due to chronic bile duct inflammation and fibrosis. Both conditions may exhibit elevated liver enzymes, but acute cholangitis tends to show a more pronounced systemic inflammatory response.
Pathophysiological Differences
Cholangitis primarily arises from bacterial infection causing inflammation and obstruction within the bile ducts, often linked to bile stasis and increased intraductal pressure. Primary sclerosing cholangitis (PSC) involves chronic immune-mediated inflammation leading to progressive fibrosis and stricturing of intrahepatic and extrahepatic bile ducts without direct infection. The key pathophysiological difference lies in cholangitis being an acute infectious process, whereas PSC represents a chronic autoimmune-mediated cholangiopathy causing bile duct scarring and cholestasis.
Diagnostic Approaches
Diagnostic approaches for acute cholangitis typically include blood tests showing elevated white blood cells, liver function abnormalities, and blood cultures to identify infectious agents. Imaging techniques such as ultrasound, magnetic resonance cholangiopancreatography (MRCP), and endoscopic retrograde cholangiopancreatography (ERCP) help visualize bile duct obstruction or inflammation. In contrast, chronic cholangitis diagnosis relies on liver biopsy, serological markers, and imaging to assess ongoing bile duct damage and fibrosis.
Key Lab Findings and Imaging
Cholangitis presents with elevated liver enzymes, particularly alkaline phosphatase and gamma-glutamyl transferase, along with leukocytosis and positive blood cultures indicating infection. Imaging studies such as ultrasound or MRCP reveal bile duct dilation and potential obstruction due to stones or strictures. In contrast, primary sclerosing cholangitis shows a cholestatic pattern with elevated alkaline phosphatase but typically lacks acute infection markers; MRCP demonstrates multifocal strictures and beading of intra- and extrahepatic bile ducts characteristic of the disease.
Treatment Strategies
Treatment strategies for cholangitis primarily involve prompt antibiotic therapy targeting common pathogens like Escherichia coli and Klebsiella species, alongside supportive care to manage sepsis and biliary obstruction. In severe cases of acute cholangitis, endoscopic retrograde cholangiopancreatography (ERCP) with biliary decompression is essential to relieve bile duct obstruction and prevent complications. Chronic cholangitis management focuses on controlling underlying causes such as primary sclerosing cholangitis through immunosuppressive agents, ursodeoxycholic acid, and liver transplantation in advanced cases.
Prognosis and Complications
Cholangitis prognosis varies significantly depending on timely diagnosis and treatment, with early-stage cases responding well to antibiotics and bile duct drainage, while delayed intervention increases risks of sepsis and liver abscesses. Complications of cholangitis include recurrent infections, biliary strictures, and secondary biliary cirrhosis, which can lead to chronic liver dysfunction and increased mortality rates. Differentiating acute cholangitis from chronic forms is critical for prognosis, as chronic cholangitis often results in progressive liver damage and higher chances of malignant transformation such as cholangiocarcinoma.
Prevention and Patient Education
Effective prevention of cholangitis centers on managing risk factors such as gallstones, bile duct obstructions, and infections through timely medical interventions and hygiene practices. Patient education emphasizes recognizing early symptoms like fever, jaundice, and abdominal pain to seek prompt treatment and avoid complications like sepsis or liver damage. Regular monitoring and lifestyle modifications, including maintaining proper hydration and avoiding biliary tract injury, enhance patient outcomes and reduce recurrence risks.
Cholangitis Infographic
 libterm.com
libterm.com