Insulinomas and glucagonomas are rare pancreatic neuroendocrine tumors that affect hormone secretion, causing significant metabolic disturbances such as hypoglycemia in insulinoma and hyperglycemia in glucagonoma. Early diagnosis and targeted treatment are crucial for managing symptoms and improving patient outcomes. Explore the rest of this article to understand how these conditions impact your health and the latest advances in their management.
Table of Comparison
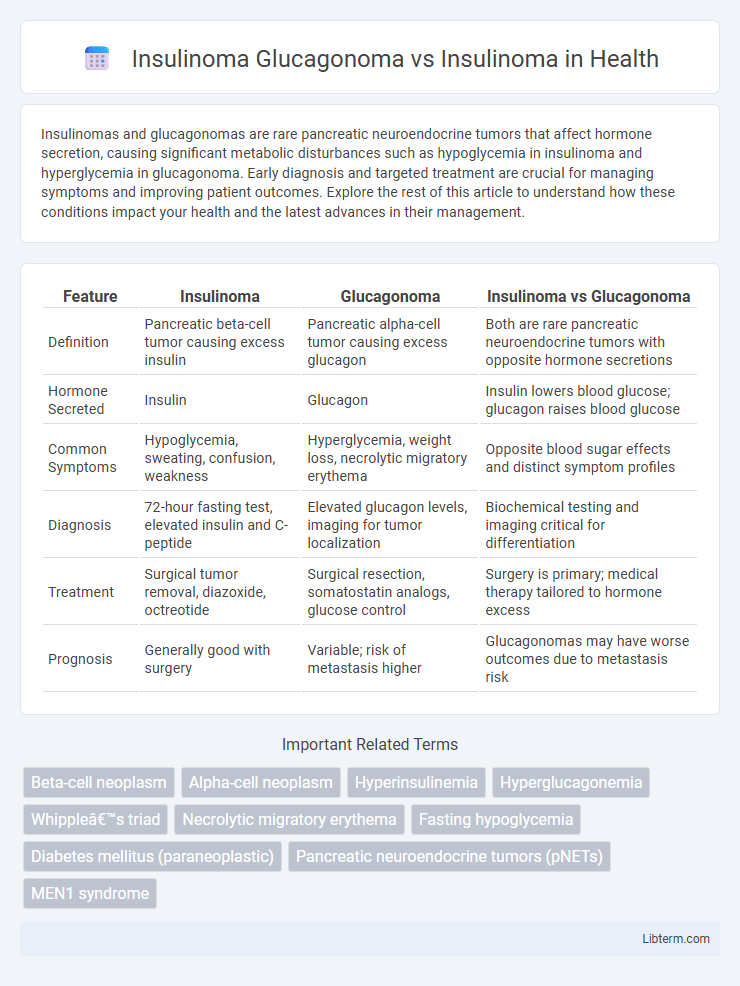
| Feature | Insulinoma | Glucagonoma | Insulinoma vs Glucagonoma |
|---|---|---|---|
| Definition | Pancreatic beta-cell tumor causing excess insulin | Pancreatic alpha-cell tumor causing excess glucagon | Both are rare pancreatic neuroendocrine tumors with opposite hormone secretions |
| Hormone Secreted | Insulin | Glucagon | Insulin lowers blood glucose; glucagon raises blood glucose |
| Common Symptoms | Hypoglycemia, sweating, confusion, weakness | Hyperglycemia, weight loss, necrolytic migratory erythema | Opposite blood sugar effects and distinct symptom profiles |
| Diagnosis | 72-hour fasting test, elevated insulin and C-peptide | Elevated glucagon levels, imaging for tumor localization | Biochemical testing and imaging critical for differentiation |
| Treatment | Surgical tumor removal, diazoxide, octreotide | Surgical resection, somatostatin analogs, glucose control | Surgery is primary; medical therapy tailored to hormone excess |
| Prognosis | Generally good with surgery | Variable; risk of metastasis higher | Glucagonomas may have worse outcomes due to metastasis risk |
Overview of Insulinoma and Glucagonoma
Insulinomas are rare neuroendocrine tumors originating in the pancreatic beta cells, causing excessive insulin secretion and resulting in hypoglycemia. Glucagonomas, also neuroendocrine tumors but arising from alpha cells of the pancreas, lead to elevated glucagon levels, often manifesting as hyperglycemia and a characteristic necrolytic migratory erythema rash. Both tumors disrupt normal glucose metabolism through hormone dysregulation but differ in clinical presentation and biochemical profile.
Etiology and Pathophysiology: Insulinoma vs Glucagonoma
Insulinomas arise from pancreatic beta cells, causing excessive insulin secretion and resulting in hypoglycemia, while glucagonomas originate from alpha cells, leading to overproduction of glucagon and hyperglycemia. Insulinoma's etiology is often sporadic but may be linked to MEN1 syndrome, whereas glucagonoma is primarily a rare neuroendocrine tumor with potential genetic predisposition. Pathophysiologically, insulinoma disrupts glucose homeostasis by increasing insulin levels independent of blood glucose, whereas glucagonoma elevates glucagon, which promotes gluconeogenesis, glycogenolysis, and lipolysis, causing characteristic clinical hyperglycemia and necrolytic migratory erythema.
Clinical Manifestations of Insulinoma
Insulinomas primarily cause hypoglycemia due to excessive insulin secretion, leading to symptoms such as confusion, sweating, palpitations, and seizures, especially during fasting or exertion. In contrast, glucagonomas are characterized by hyperglycemia, weight loss, and a distinctive rash called necrolytic migratory erythema. The clinical manifestations of insulinoma are crucial for diagnosis and differ significantly from glucagonoma, emphasizing the need for precise biochemical testing and imaging studies.
Clinical Features of Glucagonoma
Glucagonoma is characterized by a distinct clinical triad including necrolytic migratory erythema, diabetes mellitus, and weight loss, differentiating it from insulinoma which primarily causes hypoglycemia. Patients with glucagonoma often present with hyperglycemia, mild diabetes, anemia, and thromboembolic events, while insulinoma manifests with episodes of fasting hypoglycemia due to excessive insulin secretion. Elevated glucagon levels and distinctive skin lesions are key diagnostic features of glucagonoma, contrasting with the insulin-driven symptoms of insulinoma.
Key Differences: Insulinoma vs Glucagonoma
Insulinomas and glucagonomas are rare pancreatic neuroendocrine tumors that differ primarily in hormone secretion and clinical manifestations. Insulinomas secrete excess insulin, causing hypoglycemia characterized by symptoms such as confusion, sweating, and palpitations, while glucagonomas produce excess glucagon leading to hyperglycemia and a distinct rash called necrolytic migratory erythema. Diagnosis relies on biochemical tests measuring insulin or glucagon levels, with imaging techniques like CT or MRI employed for tumor localization.
Diagnostic Approaches for Insulinoma
Diagnostic approaches for insulinoma primarily involve biochemical tests such as fasting plasma glucose, insulin levels, and C-peptide measurement to confirm endogenous hyperinsulinemia. Imaging techniques including endoscopic ultrasound, CT scan, and MRI are crucial for tumor localization and differentiation from other pancreatic neuroendocrine tumors like glucagonoma. Selective arterial calcium stimulation test with hepatic venous sampling may be employed for precise localization when non-invasive imaging is inconclusive.
Diagnostic Criteria for Glucagonoma
Glucagonoma diagnosis relies on elevated plasma glucagon levels typically exceeding 500 pg/mL alongside characteristic clinical features such as necrolytic migratory erythema and weight loss. Imaging studies including CT, MRI, and somatostatin receptor scintigraphy aid in localizing the tumor. In contrast, insulinoma diagnosis is confirmed by inappropriately high insulin and C-peptide during hypoglycemia, without elevated glucagon levels, highlighting distinct biochemical profiles for these pancreatic neuroendocrine tumors.
Treatment Modalities: Insulinoma vs Glucagonoma
Treatment of insulinoma primarily involves surgical resection, which is considered the definitive cure for localized tumors, while medical management with diazoxide or somatostatin analogs like octreotide may be used preoperatively or in inoperable cases. In contrast, glucagonoma treatment emphasizes surgical removal of the pancreatic alpha-cell tumor, coupled with somatostatin analog therapy to control hormone secretion and alleviate symptoms such as necrolytic migratory erythema. Targeted therapies and chemotherapy are more commonly incorporated in malignant or metastatic cases of either insulinoma or glucagonoma, supporting symptom control and tumor burden reduction.
Prognosis and Patient Outcomes
Insulinoma typically has a favorable prognosis due to its benign nature and effective surgical removal, with cure rates exceeding 90%. Glucagonoma, although rarer and often malignant, presents a more guarded prognosis due to metastatic potential and delayed diagnosis, impacting long-term survival. Patient outcomes in insulinoma are generally positive with early detection, while glucagonoma management requires multidisciplinary treatment to address complex symptoms and tumor progression.
Summary Table: Glucagonoma vs Insulinoma
Glucagonoma and insulinoma are rare pancreatic neuroendocrine tumors with distinct hormonal secretions and clinical presentations; glucagonoma primarily secretes glucagon causing hyperglycemia, weight loss, and necrolytic migratory erythema, while insulinoma secretes insulin leading to hypoglycemia, neuroglycopenic symptoms, and adrenergic signs. Diagnosis involves biochemical assays revealing elevated glucagon levels in glucagonoma and hypoglycemia with inappropriately high insulin levels in insulinoma. Treatment typically includes surgical resection for both tumors, with somatostatin analogs used for symptom control in glucagonoma and diazoxide or frequent feeding for insulinoma-induced hypoglycemia.
Insulinoma Glucagonoma Infographic
 libterm.com
libterm.com