Pityriasis rubra pilaris is a rare chronic skin disorder characterized by reddish-orange scaling patches that often merge, causing thickened, rough skin and follicular papules. Early diagnosis and treatment are essential to manage symptoms effectively and prevent complications such as widespread skin involvement or discomfort. Explore the full article to understand the causes, symptoms, and latest treatment options for your condition.
Table of Comparison
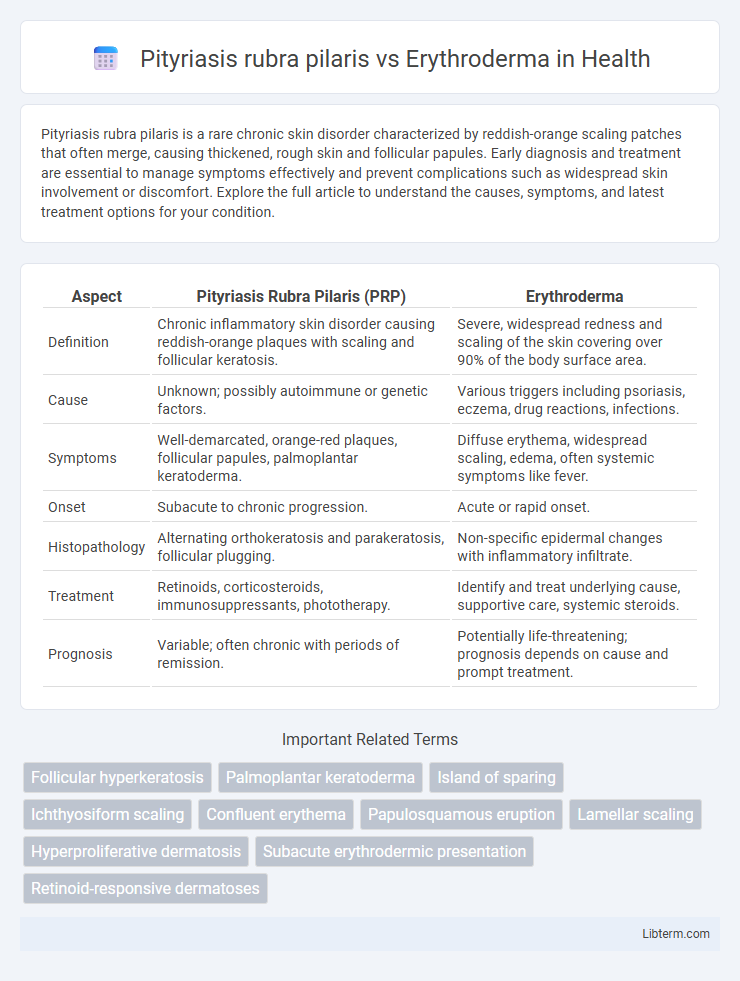
| Aspect | Pityriasis Rubra Pilaris (PRP) | Erythroderma |
|---|---|---|
| Definition | Chronic inflammatory skin disorder causing reddish-orange plaques with scaling and follicular keratosis. | Severe, widespread redness and scaling of the skin covering over 90% of the body surface area. |
| Cause | Unknown; possibly autoimmune or genetic factors. | Various triggers including psoriasis, eczema, drug reactions, infections. |
| Symptoms | Well-demarcated, orange-red plaques, follicular papules, palmoplantar keratoderma. | Diffuse erythema, widespread scaling, edema, often systemic symptoms like fever. |
| Onset | Subacute to chronic progression. | Acute or rapid onset. |
| Histopathology | Alternating orthokeratosis and parakeratosis, follicular plugging. | Non-specific epidermal changes with inflammatory infiltrate. |
| Treatment | Retinoids, corticosteroids, immunosuppressants, phototherapy. | Identify and treat underlying cause, supportive care, systemic steroids. |
| Prognosis | Variable; often chronic with periods of remission. | Potentially life-threatening; prognosis depends on cause and prompt treatment. |
Overview of Pityriasis Rubra Pilaris
Pityriasis Rubra Pilaris (PRP) is a rare chronic skin disorder characterized by reddish-orange scaly plaques, follicular hyperkeratosis, and palmoplantar keratoderma, often leading to widespread skin thickening and erythema. Unlike erythroderma, which is a severe, generalized skin inflammation involving more than 90% of the body surface area and can result from various underlying conditions, PRP has a distinctive clinical presentation and follows a more protracted course. PRP typically requires long-term management with retinoids or immunosuppressants, while erythroderma demands prompt identification and treatment of its underlying cause to prevent systemic complications.
Understanding Erythroderma
Erythroderma, a severe inflammatory skin condition characterized by widespread redness and scaling, can result from several underlying causes including Pityriasis rubra pilaris (PRP), psoriasis, and drug reactions. Differentiating erythroderma from PRP is crucial because PRP typically presents with orange-red scaling plaques and follicular hyperkeratosis, whereas erythroderma involves diffuse erythema covering more than 90% of the body surface. Timely diagnosis and management of erythroderma are essential to prevent complications such as fluid loss, temperature dysregulation, and secondary infections.
Epidemiology and Demographics
Pityriasis rubra pilaris (PRP) is a rare, chronic skin disorder with an estimated incidence of 1 in 500,000 per year, commonly affecting adults between 50 and 60 years old, with no strong gender predilection. Erythroderma, characterized by widespread erythema and scaling, has a higher incidence ranging from 1 to 2 per 100,000 population annually and is more frequently observed in middle-aged to elderly males. Both conditions show variable geographic distribution but erythroderma is often associated with underlying systemic or dermatologic diseases, influencing its epidemiological patterns.
Key Clinical Features: PRP vs Erythroderma
Pityriasis rubra pilaris (PRP) presents with well-demarcated orange-red plaques featuring follicular hyperkeratosis and islands of spared skin, whereas erythroderma involves diffuse erythema and scaling covering more than 90% of the body surface. PRP typically shows palmoplantar keratoderma and follicular plugging, contrasting with erythroderma's generalized skin redness, exfoliation, and possible systemic symptoms like fever and lymphadenopathy. Histopathology in PRP reveals alternating orthokeratosis and parakeratosis with follicular plugging, while erythroderma often shows nonspecific inflammatory patterns depending on the underlying cause.
Etiology and Pathogenesis Comparison
Pityriasis rubra pilaris (PRP) is primarily characterized by abnormal keratinization and follicular hyperkeratosis, often linked to genetic mutations in CARD14, leading to dysregulated immune responses and chronic inflammation. Erythroderma, a severe dermatologic condition, results from various etiologies including psoriasis, drug reactions, and cutaneous T-cell lymphoma, with widespread skin inflammation driven by immune dysregulation and barrier dysfunction. While PRP exhibits a distinct pathogenic mechanism centered on follicular involvement and keratinocyte abnormalities, erythroderma represents a clinical endpoint of diverse underlying diseases causing extensive epidermal inflammation and systemic immune activation.
Histopathological Differences
Pityriasis rubra pilaris (PRP) histopathology reveals alternating orthokeratosis and parakeratosis in both vertical and horizontal directions, follicular plugging, and a sparse superficial perivascular lymphohistiocytic infiltrate. In contrast, erythroderma exhibits extensive epidermal spongiosis, prominent acanthosis, and a diffuse inflammatory infiltrate without the characteristic alternating keratosis seen in PRP. These histological differences aid in distinguishing PRP from erythroderma during biopsy analysis.
Diagnostic Approach and Criteria
Pityriasis rubra pilaris (PRP) diagnosis relies on clinical presentation featuring orange-red scaly plaques with islands of sparing and follicular hyperkeratosis, supported by histopathology showing alternating orthokeratosis and parakeratosis. Erythroderma diagnosis requires identifying generalized erythema involving over 90% of the body surface area, with causes ranging from psoriasis, drug reactions, or cutaneous T-cell lymphoma, confirmed by skin biopsy and laboratory tests to exclude systemic involvement. Skin biopsy remains critical in differentiating PRP's characteristic vertical and horizontal epidermal changes from the diffuse epidermal and inflammatory infiltrate seen in erythroderma.
Treatment Modalities: PRP vs Erythroderma
Pityriasis rubra pilaris (PRP) treatment primarily involves systemic retinoids such as acitretin and immunosuppressants like methotrexate to reduce hyperkeratosis and inflammation. In contrast, erythroderma requires prompt identification of underlying causes followed by supportive care including fluid and electrolyte management, topical corticosteroids, and systemic therapies tailored to the etiology, such as immunosuppressants or biologics. Targeted therapies for PRP focus on modulating keratinization, whereas erythroderma treatment emphasizes stabilizing skin barrier function and controlling systemic complications.
Prognosis and Disease Course
Pityriasis rubra pilaris (PRP) typically follows a chronic, relapsing course with variable prognosis, where classic adult forms can persist for several years but often improve with treatment, while juvenile types may resolve spontaneously. Erythroderma, characterized by widespread redness and scaling, usually presents as a severe, acute condition with a more guarded prognosis due to potential complications such as infections, fluid imbalance, and systemic involvement. Prognosis in erythroderma largely depends on prompt diagnosis and management of underlying causes, whereas PRP prognosis varies based on subtype and response to therapies.
Clinical Pearls: Distinguishing PRP from Erythroderma
Pityriasis rubra pilaris (PRP) often presents with well-demarcated, orange-red plaques, follicular hyperkeratosis, and islands of sparing, which are key clinical pearls distinguishing it from erythroderma, where diffuse erythema and scaling typically involve nearly 90% or more of the body surface area. PRP exhibits follicular-based papules and a characteristic "nutmeg grater" feel on affected skin, while erythroderma manifests as widespread redness and desquamation without follicular prominence. Recognition of these features aids in differentiating PRP from erythroderma, directing appropriate diagnostic evaluation and management strategies.
Pityriasis rubra pilaris Infographic
 libterm.com
libterm.com