Airway hyperresponsiveness is a condition where the airways overreact to various stimuli, leading to narrowing and difficulty breathing. This heightened sensitivity is commonly seen in asthma and other respiratory disorders, impacting your lung function and overall health. Discover more about the causes, symptoms, and treatments in the rest of the article.
Table of Comparison
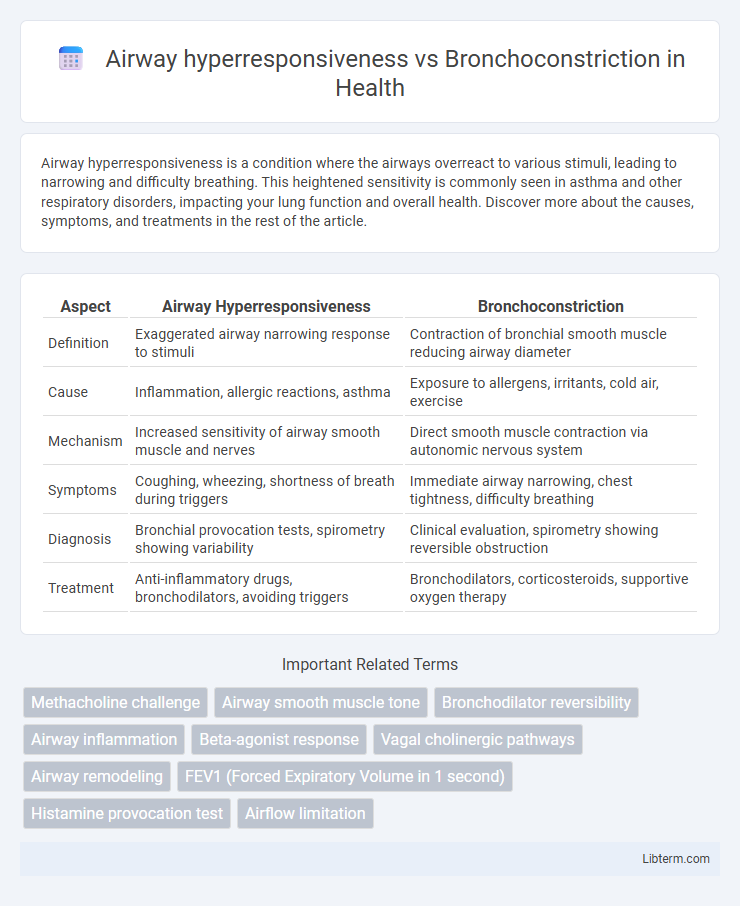
| Aspect | Airway Hyperresponsiveness | Bronchoconstriction |
|---|---|---|
| Definition | Exaggerated airway narrowing response to stimuli | Contraction of bronchial smooth muscle reducing airway diameter |
| Cause | Inflammation, allergic reactions, asthma | Exposure to allergens, irritants, cold air, exercise |
| Mechanism | Increased sensitivity of airway smooth muscle and nerves | Direct smooth muscle contraction via autonomic nervous system |
| Symptoms | Coughing, wheezing, shortness of breath during triggers | Immediate airway narrowing, chest tightness, difficulty breathing |
| Diagnosis | Bronchial provocation tests, spirometry showing variability | Clinical evaluation, spirometry showing reversible obstruction |
| Treatment | Anti-inflammatory drugs, bronchodilators, avoiding triggers | Bronchodilators, corticosteroids, supportive oxygen therapy |
Introduction to Airway Hyperresponsiveness and Bronchoconstriction
Airway hyperresponsiveness is a heightened sensitivity of the airways to various stimuli, leading to exaggerated bronchoconstriction. Bronchoconstriction refers to the narrowing of the airways caused by the contraction of smooth muscle surrounding the bronchi. Understanding the distinction is crucial in diagnosing and managing respiratory conditions such as asthma and chronic obstructive pulmonary disease (COPD).
Defining Airway Hyperresponsiveness
Airway hyperresponsiveness (AHR) is characterized by an exaggerated bronchoconstrictive response of the airways to various stimuli, such as allergens, cold air, or exercise, which is a hallmark feature of asthma. Unlike bronchoconstriction, which refers specifically to the narrowing of the airways due to smooth muscle contraction, AHR reflects an overall increased sensitivity and reactivity of the airway tissues leading to exaggerated bronchoconstriction. This enhanced responsiveness results from inflammation, structural changes, and epithelial dysfunction within the airways that amplify the airway narrowing response.
Understanding Bronchoconstriction
Bronchoconstriction refers to the narrowing of airways due to the tightening of surrounding smooth muscle, often triggered by allergens, irritants, or inflammation. This physiological response reduces airflow and contributes to symptoms such as wheezing, coughing, and shortness of breath in conditions like asthma and chronic obstructive pulmonary disease (COPD). Distinguishing bronchoconstriction from airway hyperresponsiveness, which is an exaggerated bronchoconstrictive response to various stimuli, is essential for targeted therapeutic interventions.
Pathophysiological Differences
Airway hyperresponsiveness (AHR) is characterized by an exaggerated bronchoconstrictive response to various stimuli, primarily due to heightened airway smooth muscle sensitivity and chronic airway inflammation involving eosinophils and mast cells. Bronchoconstriction directly refers to the narrowing of airways caused by contraction of the airway smooth muscle, often triggered by acute exposure to allergens, irritants, or parasympathetic nervous system activation. Pathophysiologically, AHR reflects an underlying chronic inflammatory state and structural airway remodeling, whereas bronchoconstriction represents the acute functional change without necessarily involving long-term airway alteration.
Underlying Mechanisms and Triggers
Airway hyperresponsiveness involves an exaggerated bronchoconstrictive response to various stimuli due to inflammation-driven airway remodeling, increased smooth muscle mass, and heightened neural reflexes. Bronchoconstriction occurs when airway smooth muscle contracts, narrowing the airways, primarily triggered by allergens, irritants, cold air, or exercise-induced reflexes. The underlying mechanisms include mast cell activation releasing histamines and leukotrienes, as well as autonomic nervous system imbalance enhancing airway smooth muscle sensitivity.
Clinical Manifestations and Symptoms
Airway hyperresponsiveness is characterized by an exaggerated bronchoconstrictive response to various stimuli, leading to symptoms such as wheezing, coughing, chest tightness, and shortness of breath, commonly observed in asthma patients. Bronchoconstriction refers to the actual narrowing of the airways due to contraction of smooth muscles, resulting in airflow limitation and respiratory distress. Clinically, both conditions manifest with similar respiratory symptoms, but airway hyperresponsiveness is a predisposition that causes bronchoconstriction episodes upon exposure to triggers like allergens, cold air, or exercise.
Diagnostic Approaches
Airway hyperresponsiveness (AHR) is diagnosed through bronchoprovocation tests such as methacholine or histamine challenge, measuring the degree of airway narrowing in response to specific stimuli. Bronchoconstriction is assessed using spirometry to evaluate changes in airflow, particularly reductions in FEV1 after exposure to allergens, irritants, or exercise. Combining these diagnostic approaches provides a comprehensive evaluation of airway sensitivity and airflow limitation in respiratory conditions like asthma.
Treatment and Management Strategies
Treatment strategies for airway hyperresponsiveness primarily involve long-term control medications such as inhaled corticosteroids and leukotriene modifiers to reduce airway inflammation and sensitivity. Bronchoconstriction management focuses on rapid relief using short-acting beta-agonists like albuterol to relax airway smooth muscle during acute episodes. Combining anti-inflammatory therapies with bronchodilators optimizes control of symptoms and prevents exacerbations in conditions like asthma.
Airway Hyperresponsiveness vs Bronchoconstriction: Key Differences
Airway hyperresponsiveness (AHR) is a heightened sensitivity of the airways to various stimuli, leading to exaggerated bronchoconstriction, whereas bronchoconstriction refers specifically to the narrowing of the airways due to smooth muscle contraction. AHR is a pathological condition often associated with asthma and chronic obstructive pulmonary disease (COPD), characterized by an increased response to allergens, irritants, or cold air, while bronchoconstriction is a physiological response that can occur in various respiratory conditions. Understanding the distinction between AHR as an exaggerated airway sensitivity and bronchoconstriction as the resulting airway narrowing is critical for accurate diagnosis and targeted therapeutic interventions.
Future Perspectives and Research Directions
Future perspectives in airway hyperresponsiveness and bronchoconstriction research emphasize the development of targeted molecular therapies that modulate smooth muscle contraction and inflammatory signaling pathways. Advances in precision medicine and biomarker identification aim to enable personalized treatment strategies for asthma and COPD patients with distinct hyperresponsive phenotypes. Emerging technologies such as single-cell RNA sequencing and organ-on-a-chip models hold potential to unravel cellular mechanisms underlying hyperresponsiveness, facilitating novel drug discovery and improved clinical outcomes.
Airway hyperresponsiveness Infographic
 libterm.com
libterm.com