Pancreatitis is a condition characterized by inflammation of the pancreas, causing severe abdominal pain and digestive issues. Managing this disorder often requires dietary changes, medication, or in severe cases, hospitalization to prevent complications. Discover effective treatments and lifestyle tips to protect your pancreas by reading the full article.
Table of Comparison
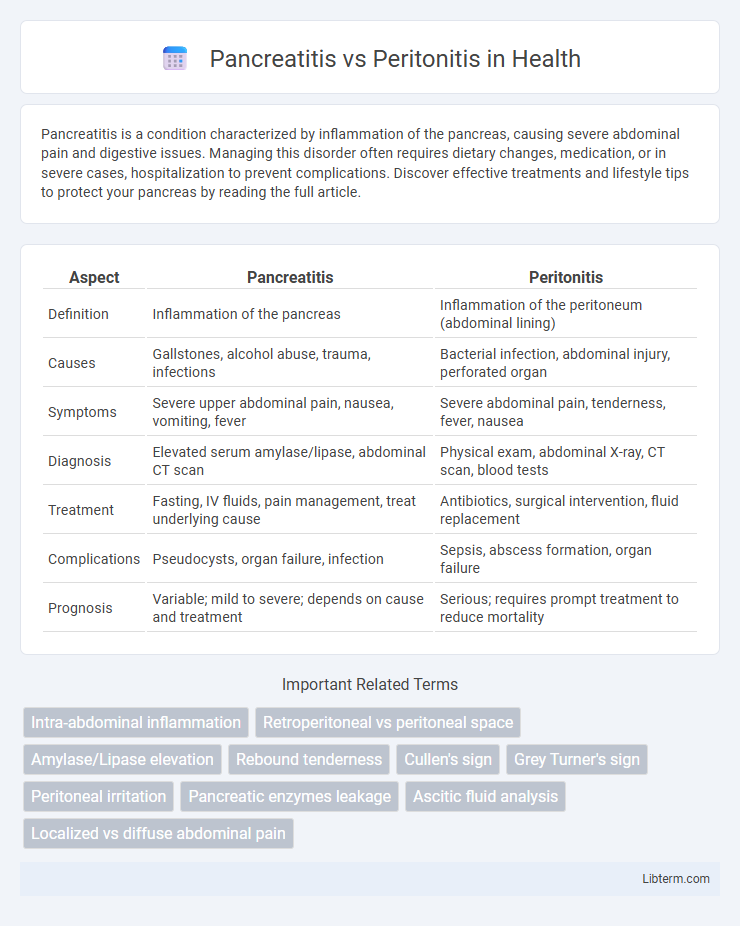
| Aspect | Pancreatitis | Peritonitis |
|---|---|---|
| Definition | Inflammation of the pancreas | Inflammation of the peritoneum (abdominal lining) |
| Causes | Gallstones, alcohol abuse, trauma, infections | Bacterial infection, abdominal injury, perforated organ |
| Symptoms | Severe upper abdominal pain, nausea, vomiting, fever | Severe abdominal pain, tenderness, fever, nausea |
| Diagnosis | Elevated serum amylase/lipase, abdominal CT scan | Physical exam, abdominal X-ray, CT scan, blood tests |
| Treatment | Fasting, IV fluids, pain management, treat underlying cause | Antibiotics, surgical intervention, fluid replacement |
| Complications | Pseudocysts, organ failure, infection | Sepsis, abscess formation, organ failure |
| Prognosis | Variable; mild to severe; depends on cause and treatment | Serious; requires prompt treatment to reduce mortality |
Understanding Pancreatitis and Peritonitis
Pancreatitis is inflammation of the pancreas caused by factors such as gallstones, alcohol abuse, or trauma, presenting with severe abdominal pain and elevated pancreatic enzymes. Peritonitis involves inflammation of the peritoneum, often due to infection or perforation of abdominal organs, leading to widespread abdominal tenderness and systemic symptoms like fever and sepsis. Accurate diagnosis relies on imaging studies like CT scans and laboratory tests including serum amylase for pancreatitis and peritoneal fluid analysis for peritonitis.
Causes and Risk Factors
Pancreatitis primarily arises from gallstones obstructing the pancreatic duct and chronic alcohol consumption damaging pancreatic tissue. Peritonitis is commonly caused by bacterial infection due to a perforated abdominal organ, such as a ruptured appendix or perforated ulcer. Risk factors for pancreatitis include high triglyceride levels and certain medications, while peritonitis risk increases with abdominal surgery, trauma, or conditions leading to gastrointestinal perforation.
Symptoms Comparison: Pancreatitis vs Peritonitis
Pancreatitis presents with severe upper abdominal pain radiating to the back, accompanied by nausea, vomiting, and elevated pancreatic enzymes like amylase and lipase. Peritonitis typically manifests as widespread abdominal tenderness, guarding, rebound pain, fever, and signs of systemic infection such as tachycardia and hypotension. Distinguishing these conditions relies on clinical evaluation and diagnostic imaging, with pancreatitis showing localized inflammation and peritonitis indicating diffuse peritoneal irritation.
Diagnostic Methods
Pancreatitis diagnosis primarily relies on elevated serum amylase and lipase levels combined with abdominal ultrasound or contrast-enhanced computed tomography (CT) to assess pancreatic inflammation. Peritonitis diagnosis involves analysis of peritoneal fluid obtained via paracentesis, revealing elevated white blood cells and bacterial cultures, supplemented by abdominal X-rays or CT scans detecting free air or fluid. Both conditions require accurate imaging and laboratory tests to differentiate the source of abdominal pain effectively.
Key Differences in Pathophysiology
Pancreatitis involves inflammation of the pancreas caused by premature activation of pancreatic enzymes, leading to autodigestion and tissue damage. Peritonitis is characterized by inflammation of the peritoneum, often resulting from infection, perforation, or leakage of abdominal contents into the peritoneal cavity. While pancreatitis primarily affects pancreatic tissue disrupting enzyme regulation, peritonitis impacts the peritoneal lining causing widespread abdominal inflammation and systemic infection.
Common Complications
Pancreatitis commonly leads to complications such as pancreatic pseudocysts, necrosis, and systemic inflammatory response syndrome (SIRS), which can progress to multi-organ failure. Peritonitis often results in abscess formation, sepsis, and widespread infection causing peritoneal adhesions and sepsis-induced organ dysfunction. Both conditions require prompt medical intervention to prevent severe morbidity and mortality associated with their complications.
Treatment Approaches
Treatment approaches for pancreatitis primarily involve fasting to rest the pancreas, intravenous fluids for hydration, pain management, and addressing the underlying cause such as gallstones or alcohol use; severe cases may require surgery or endoscopic intervention. Peritonitis treatment centers on prompt administration of broad-spectrum antibiotics to combat infection, surgical intervention to repair the source of contamination like a perforated organ, and supportive care including fluid replacement and pain control. Early diagnosis and targeted therapy are critical in both conditions to prevent systemic complications such as sepsis and multi-organ failure.
Prognosis and Long-Term Outcomes
Pancreatitis carries a variable prognosis depending on its severity, with mild cases resolving fully and severe acute pancreatitis associated with complications such as necrosis and organ failure, potentially leading to chronic pancreatitis and long-term pancreatic insufficiency. Peritonitis prognosis depends on the underlying cause and timeliness of treatment; bacterial peritonitis often requires prompt antibiotics and surgical intervention, with delayed management increasing risks of sepsis and mortality. Long-term outcomes for patients surviving peritonitis may include adhesions and chronic abdominal pain, whereas chronic pancreatitis frequently results in persistent pain, malabsorption, and diabetes mellitus due to sustained pancreatic damage.
Preventive Measures and Lifestyle Modifications
Preventive measures for pancreatitis include avoiding excessive alcohol consumption, maintaining a balanced diet low in fat, and managing underlying conditions like gallstones and hypertriglyceridemia. For peritonitis, prevention centers on timely treatment of abdominal infections, proper sterilization during surgeries, and managing conditions such as appendicitis or abdominal trauma. Lifestyle modifications promoting overall digestive health, safe food handling, and regular medical check-ups reduce the risk of both pancreatitis and peritonitis.
When to Seek Medical Attention
Severe abdominal pain persisting for more than a few hours, accompanied by fever, vomiting, or swelling, signals the need for immediate medical evaluation to distinguish between pancreatitis and peritonitis. Signs such as rapid heartbeat, low blood pressure, or signs of shock require emergency care due to the life-threatening nature of these conditions. Early diagnosis and treatment are crucial to prevent complications like organ failure or sepsis.
Pancreatitis Infographic
 libterm.com
libterm.com