Psoriasis is a chronic autoimmune condition characterized by rapid skin cell turnover, leading to red, scaly patches that can cause discomfort and affect your confidence. Effective management hinges on understanding triggers and incorporating topical treatments, phototherapy, or systemic medications tailored to your symptoms. Discover comprehensive strategies to alleviate psoriasis and improve your skin's health by reading the full article.
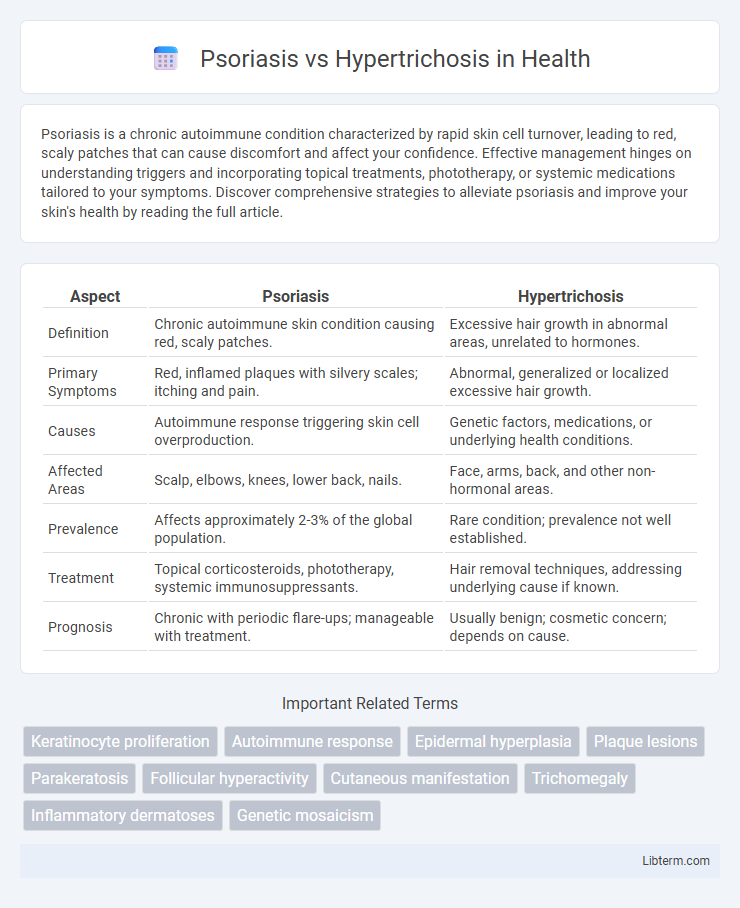
Table of Comparison
| Aspect | Psoriasis | Hypertrichosis |
|---|---|---|
| Definition | Chronic autoimmune skin condition causing red, scaly patches. | Excessive hair growth in abnormal areas, unrelated to hormones. |
| Primary Symptoms | Red, inflamed plaques with silvery scales; itching and pain. | Abnormal, generalized or localized excessive hair growth. |
| Causes | Autoimmune response triggering skin cell overproduction. | Genetic factors, medications, or underlying health conditions. |
| Affected Areas | Scalp, elbows, knees, lower back, nails. | Face, arms, back, and other non-hormonal areas. |
| Prevalence | Affects approximately 2-3% of the global population. | Rare condition; prevalence not well established. |
| Treatment | Topical corticosteroids, phototherapy, systemic immunosuppressants. | Hair removal techniques, addressing underlying cause if known. |
| Prognosis | Chronic with periodic flare-ups; manageable with treatment. | Usually benign; cosmetic concern; depends on cause. |
Understanding Psoriasis: Causes and Symptoms
Psoriasis is a chronic autoimmune skin condition characterized by the rapid buildup of skin cells, leading to thick, red, scaly patches often found on the elbows, knees, and scalp. Its primary causes include genetic predisposition, immune system dysfunction, and environmental triggers such as stress or infections. Symptoms of psoriasis vary from mild to severe and commonly involve itching, burning sensations, and cracked skin, distinguishing it from hypertrichosis, which primarily entails abnormal hair growth without skin inflammation.
What is Hypertrichosis? Key Features Explained
Hypertrichosis is a rare condition characterized by excessive hair growth on areas of the body where hair is normally minimal or absent, distinguishing it from typical hair patterns seen in psoriasis, which primarily involves skin inflammation and scaling. Key features of hypertrichosis include generalized or localized abnormal hair growth that can be congenital or acquired due to genetic factors, medications, or systemic disorders. Unlike psoriasis, which presents with red, scaly plaques and can affect skin texture and appearance, hypertrichosis is primarily diagnosed by the presence of dense, thick hair covering unusual regions without associated inflammation.
Psoriasis vs Hypertrichosis: Distinguishing Clinical Manifestations
Psoriasis presents with well-demarcated, erythematous plaques covered by silvery-white scales, primarily affecting extensor surfaces like elbows and knees, whereas hypertrichosis involves excessive hair growth beyond age, sex, or race norms without inflammatory skin changes. Psoriatic lesions often exhibit Auspitz sign and nail pitting, aiding clinical diagnosis, while hypertrichosis lacks such epidermal or nail involvement. Recognizing these distinctions is crucial for accurate diagnosis and targeted treatment strategies.
Genetic and Environmental Triggers
Psoriasis is primarily influenced by genetic predisposition involving HLA-Cw6 alleles combined with environmental triggers such as stress, infections, and skin injury, leading to immune system dysregulation and chronic inflammation. Hypertrichosis, often caused by genetic mutations affecting hair growth cycles or as a side effect of medications, can also result from environmental factors like exposure to certain toxins or hormonal imbalances. Understanding the genetic markers and external triggers in both conditions is essential for targeted therapeutic strategies and personalized treatment plans.
Diagnostic Approaches: How Specialists Differentiate
Dermatologists differentiate psoriasis from hypertrichosis through distinct diagnostic methods, including clinical examination and patient history review. Psoriasis is identified by characteristic erythematous plaques with silvery scales, often confirmed by a skin biopsy revealing epidermal hyperplasia and inflammatory infiltration. Conversely, hypertrichosis diagnosis relies on observation of excessive hair growth patterns without inflammatory signs, possibly supplemented by hormonal or genetic testing to determine underlying causes.
Typical Treatment Strategies for Psoriasis
Psoriasis treatment typically involves topical corticosteroids, vitamin D analogs, and phototherapy to reduce inflammation and slow skin cell growth. Systemic therapies such as methotrexate, cyclosporine, and biologics like tumor necrosis factor (TNF) inhibitors target severe or resistant cases. Unlike hypertrichosis, which focuses on hair removal methods, psoriasis management centers on immune modulation and skin repair.
Managing Hypertrichosis: Options and Considerations
Managing hypertrichosis involves various options such as laser hair removal, electrolysis, and prescription topical treatments like eflornithine cream to reduce unwanted hair growth effectively. Patient considerations include hair color, skin type, underlying causes, and potential side effects, making individualized treatment plans essential. Consistent follow-up and combination therapies often improve outcomes in hypertrichosis management compared to single-method approaches.
Quality of Life: Patient Experiences Compared
Psoriasis significantly impacts quality of life due to chronic skin inflammation, visible plaques, and associated itching or pain, often leading to social embarrassment and emotional distress. Hypertrichosis, characterized by excessive hair growth, primarily affects self-esteem and social interactions, with psychological challenges tied to altered appearance rather than physical discomfort. Both conditions require tailored psychosocial support strategies, but psoriasis patients frequently report greater physical symptom burden and quality-of-life impairment compared to those with hypertrichosis.
Common Myths and Misconceptions
Psoriasis is often mistakenly believed to be contagious or caused by poor hygiene, while hypertrichosis is commonly thought to result solely from hormonal imbalances, despite genetic and medication-related causes. Many assume psoriasis only affects the skin, not realizing it can involve systemic inflammation and joint symptoms as seen in psoriatic arthritis. Hypertrichosis is frequently confused with hirsutism, yet it refers to excessive hair growth regardless of gender or androgen levels, differentiating it from the hormone-related condition.
When to Seek Medical Advice
Seek medical advice for psoriasis when experiencing persistent red, scaly patches that cause itching, pain, or bleeding, as early treatment can prevent worsening and complications like psoriatic arthritis. In cases of hypertrichosis, consult a healthcare provider if there is sudden, excessive hair growth in unusual patterns or areas, which may indicate underlying hormonal imbalances or systemic conditions. Timely medical evaluation helps determine the appropriate diagnosis and management for both chronic skin inflammation and abnormal hair growth disorders.
Psoriasis Infographic
 libterm.com
libterm.com