Oral candidiasis is a common fungal infection caused by the overgrowth of Candida species, primarily Candida albicans, in the mouth. Symptoms include white patches on the tongue or inner cheeks, soreness, and difficulty swallowing, often affecting individuals with weakened immune systems or those using certain medications. Explore the full article to understand the causes, symptoms, and effective treatments for managing oral candidiasis.
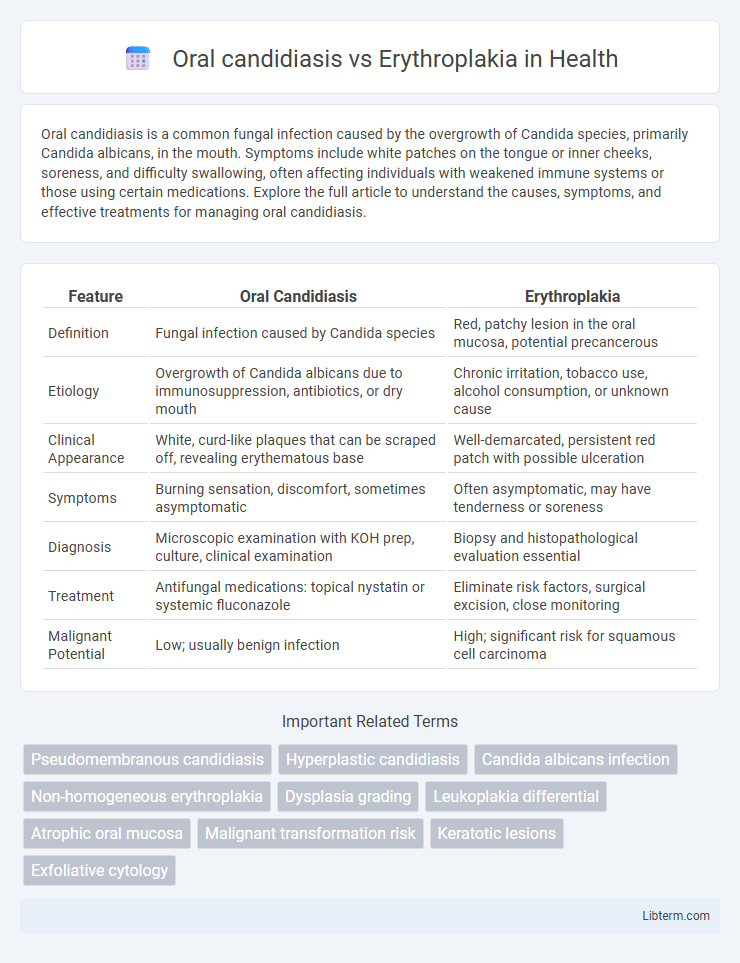
Table of Comparison
| Feature | Oral Candidiasis | Erythroplakia |
|---|---|---|
| Definition | Fungal infection caused by Candida species | Red, patchy lesion in the oral mucosa, potential precancerous |
| Etiology | Overgrowth of Candida albicans due to immunosuppression, antibiotics, or dry mouth | Chronic irritation, tobacco use, alcohol consumption, or unknown cause |
| Clinical Appearance | White, curd-like plaques that can be scraped off, revealing erythematous base | Well-demarcated, persistent red patch with possible ulceration |
| Symptoms | Burning sensation, discomfort, sometimes asymptomatic | Often asymptomatic, may have tenderness or soreness |
| Diagnosis | Microscopic examination with KOH prep, culture, clinical examination | Biopsy and histopathological evaluation essential |
| Treatment | Antifungal medications: topical nystatin or systemic fluconazole | Eliminate risk factors, surgical excision, close monitoring |
| Malignant Potential | Low; usually benign infection | High; significant risk for squamous cell carcinoma |
Introduction to Oral Candidiasis and Erythroplakia
Oral candidiasis is a fungal infection caused by Candida species, primarily Candida albicans, presenting as white, creamy lesions on the mucosal surfaces that can be scraped off, commonly affecting immunocompromised individuals. Erythroplakia manifests as a red, velvety patch on the oral mucosa with a high risk of dysplasia or malignancy, often requiring biopsy for definitive diagnosis. Both conditions necessitate prompt evaluation to differentiate between infectious and potentially premalignant lesions in the oral cavity.
Etiology and Risk Factors
Oral candidiasis is primarily caused by the overgrowth of Candida species, particularly Candida albicans, often triggered by immunosuppression, antibiotic use, diabetes, or xerostomia. Erythroplakia, a potentially malignant lesion, arises mainly due to chronic irritation from tobacco use, alcohol consumption, and human papillomavirus (HPV) infection. Both conditions share risk factors such as smoking and immunocompromised states but differ fundamentally in their etiology, with candidiasis being infectious and erythroplakia linked to epithelial dysplasia and carcinogenic exposure.
Pathophysiology: Fungal vs. Epithelial Lesions
Oral candidiasis arises from an overgrowth of the Candida species, primarily Candida albicans, leading to fungal infection characterized by white pseudomembranous plaques and mucosal inflammation due to fungal hyphae penetration. Erythroplakia, in contrast, represents a premalignant epithelial lesion marked by dysplastic changes and angiogenesis within the oral mucosa, exhibiting erythematous, velvety patches without fungal involvement. The pathophysiology of oral candidiasis centers on fungal invasion and host immune response, whereas erythroplakia involves epithelial atypia and potential malignant transformation driven by genetic mutations and altered cellular proliferation.
Clinical Presentation and Key Differences
Oral candidiasis presents as white, curd-like plaques on the mucosal surfaces that can be wiped off, often accompanied by erythema and discomfort, primarily caused by Candida albicans overgrowth. Erythroplakia appears as a persistent, sharply demarcated, red patch on the oral mucosa that cannot be scraped off and is strongly associated with dysplasia or carcinoma in situ. Key differences include the lesion's color, texture, and response to antifungal treatment, with oral candidiasis showing reversibility and erytheplakia requiring biopsy due to its high malignant potential.
Diagnostic Criteria and Techniques
Oral candidiasis diagnosis relies on clinical presentation such as white pseudomembranous plaques and confirmed through potassium hydroxide (KOH) preparation or fungal culture to identify Candida albicans. Erythroplakia requires biopsy and histopathological examination revealing epithelial dysplasia or carcinoma in situ, as its clinical appearance is a sharply demarcated, velvety erythematous patch with no specific pathogen. Advanced imaging techniques like autofluorescence and toluidine blue staining assist in delineating lesion margins, improving diagnostic accuracy for erythroplakia compared to fungal tests used in oral candidiasis.
Histopathological Features
Oral candidiasis histopathology reveals superficial epithelial infection with pseudohyphae and yeast cells infiltrating the keratin layer, accompanied by inflammatory cell infiltration. In contrast, erythroplakia exhibits dysplastic epithelial changes including disorganized basal cell layers, nuclear pleomorphism, and increased mitotic figures without fungal presence. The distinct histopathological markers aid in differentiating fungal infection from potentially premalignant epithelial alterations.
Differential Diagnosis
Oral candidiasis presents as white, curd-like plaques that can be wiped off, often revealing erythematous mucosa, whereas erythroplakia manifests as persistent, well-demarcated red patches that cannot be scraped off. Differential diagnosis relies on clinical examination, cytological smear, and histopathological biopsy to distinguish fungal infection in candidiasis from epithelial dysplasia or carcinoma in erythroplakia. Microbiological culture confirms Candida species, whereas biopsy is crucial for erythroplakia due to its high malignant transformation risk.
Treatment Strategies and Management
Oral candidiasis treatment primarily involves antifungal agents such as nystatin, clotrimazole troches, or systemic fluconazole for severe cases, with emphasis on managing underlying risk factors like immunosuppression or antibiotic use. Erythroplakia requires prompt biopsy and histopathological examination due to its high malignant transformation potential, followed by surgical excision or laser therapy for confirmed dysplasia or carcinoma in situ. Regular monitoring and patient education on risk factor modification, including tobacco cessation, are critical components in managing both conditions effectively.
Prognosis and Malignant Potential
Oral candidiasis typically has an excellent prognosis with proper antifungal treatment and minimal risk of malignant transformation, as it is a fungal infection rather than a precancerous lesion. In contrast, erythroplakia carries a significant malignant potential, with studies indicating up to 90% of cases showing dysplasia or carcinoma in situ upon biopsy, necessitating close monitoring and often surgical intervention. Early detection and histopathological evaluation of erythroplakia are critical for improving patient outcomes due to its high risk of progression to oral squamous cell carcinoma.
Prevention and Patient Education
Oral candidiasis prevention centers on maintaining good oral hygiene, managing underlying conditions like diabetes, and proper use of antifungal medications to reduce fungal overgrowth. For erythroplakia, patient education emphasizes avoiding tobacco and alcohol, regular dental check-ups, and prompt evaluation of any persistent red patches for early detection of potential precancerous changes. Educating patients about lifestyle modifications and symptom awareness is crucial to reducing the risk and improving outcomes for both conditions.
Oral candidiasis Infographic
 libterm.com
libterm.com