Hepatitis is a liver inflammation caused by viral infections, toxins, or autoimmune conditions, leading to symptoms like fatigue, jaundice, and abdominal pain. Early diagnosis and treatment are crucial to prevent severe liver damage or chronic disease. Discover more about hepatitis types, symptoms, prevention, and treatment options in the rest of the article.
Table of Comparison
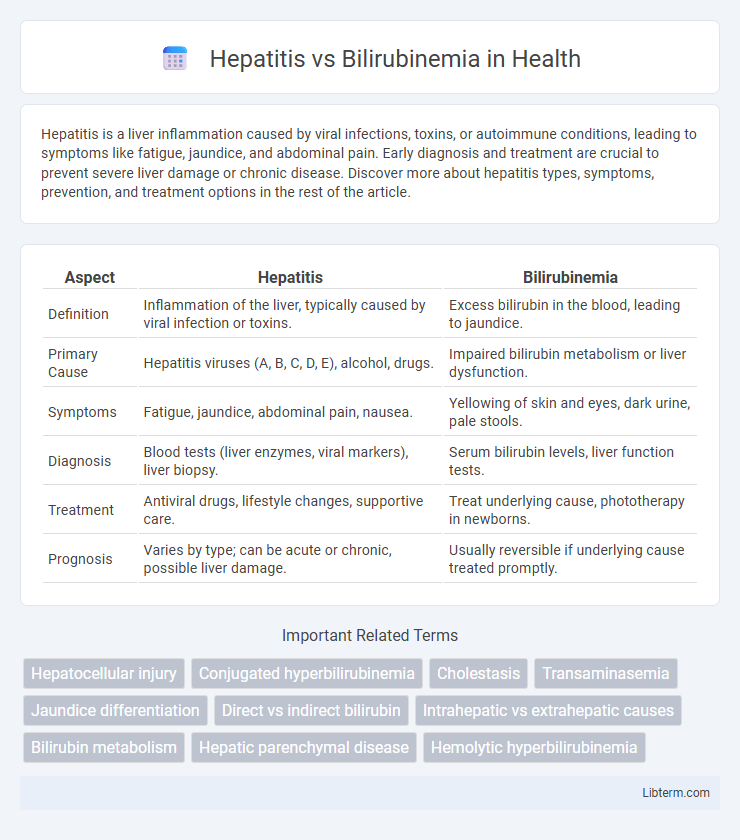
| Aspect | Hepatitis | Bilirubinemia |
|---|---|---|
| Definition | Inflammation of the liver, typically caused by viral infection or toxins. | Excess bilirubin in the blood, leading to jaundice. |
| Primary Cause | Hepatitis viruses (A, B, C, D, E), alcohol, drugs. | Impaired bilirubin metabolism or liver dysfunction. |
| Symptoms | Fatigue, jaundice, abdominal pain, nausea. | Yellowing of skin and eyes, dark urine, pale stools. |
| Diagnosis | Blood tests (liver enzymes, viral markers), liver biopsy. | Serum bilirubin levels, liver function tests. |
| Treatment | Antiviral drugs, lifestyle changes, supportive care. | Treat underlying cause, phototherapy in newborns. |
| Prognosis | Varies by type; can be acute or chronic, possible liver damage. | Usually reversible if underlying cause treated promptly. |
Understanding Hepatitis: Causes and Types
Hepatitis refers to inflammation of the liver caused by viral infections such as Hepatitis A, B, C, D, and E, with each type differing in transmission methods and severity. Causes extend beyond viruses to include alcohol abuse, autoimmune diseases, and certain medications, all leading to liver damage. Distinguishing hepatitis from bilirubinemia, a condition characterized by excess bilirubin in the blood causing jaundice, is crucial for accurate diagnosis and treatment.
What is Bilirubinemia? Definition and Overview
Bilirubinemia refers to an elevated level of bilirubin in the bloodstream, which is a yellow pigment produced during the normal breakdown of red blood cells. This condition often results in jaundice, characterized by yellowing of the skin and eyes, and can indicate underlying liver dysfunction or hemolytic disorders. Unlike hepatitis, which is an inflammation of the liver often caused by viral infection, bilirubinemia is a biochemical condition signaling impaired bilirubin metabolism or clearance.
Key Differences Between Hepatitis and Bilirubinemia
Hepatitis is an inflammation of the liver caused by viral infections, toxins, or autoimmune diseases, leading to symptoms such as jaundice, fatigue, and abdominal pain. Bilirubinemia refers to the elevated levels of bilirubin in the blood, often resulting from liver dysfunction, hemolysis, or bile duct obstruction, and primarily causes jaundice and dark urine. The key difference is that hepatitis is an underlying liver condition causing inflammation, while bilirubinemia is a biochemical condition indicating excess bilirubin, which may result from hepatitis or other hepatic and hematologic disorders.
Clinical Symptoms: Comparing Hepatitis and Bilirubinemia
Hepatitis commonly presents with symptoms such as fatigue, jaundice, dark urine, and abdominal pain, primarily due to liver inflammation and damage. Bilirubinemia, characterized by elevated bilirubin levels, mainly causes jaundice and may lead to dark urine and pale stools without significant systemic symptoms. Differentiating these conditions clinically relies on identifying additional signs like hepatomegaly and elevated liver enzymes in hepatitis versus isolated bilirubin elevation in bilirubinemia.
Diagnostic Approaches for Hepatitis vs Bilirubinemia
Hepatitis diagnosis primarily relies on serological tests such as hepatitis virus-specific antibodies (Anti-HAV, HBsAg, Anti-HCV) and liver function tests indicating elevated ALT and AST levels. Bilirubinemia diagnosis involves measuring total and direct bilirubin in serum to distinguish between unconjugated and conjugated hyperbilirubinemia, alongside imaging studies like ultrasound to assess biliary obstruction. Liver biopsy may be utilized in hepatitis for histopathological confirmation, whereas bilirubinemia often requires further evaluation of hemolytic markers (e.g., reticulocyte count) to identify underlying causes.
Underlying Risk Factors for Each Condition
Hepatitis risk factors primarily include viral infections (hepatitis A, B, C viruses), excessive alcohol consumption, and exposure to hepatotoxic drugs or toxins. Bilirubinemia, often resulting in jaundice, is commonly associated with hemolytic disorders, liver dysfunction, or bile duct obstruction leading to impaired bilirubin metabolism. Understanding these distinct underlying causes is crucial for accurate diagnosis and targeted treatment of each condition.
Laboratory Markers: Hepatitis vs Bilirubinemia
Hepatitis typically presents with elevated liver enzymes such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), indicating hepatocellular injury, whereas bilirubinemia primarily shows increased total and direct bilirubin levels due to impaired bilirubin metabolism or excretion. In hepatitis, alkaline phosphatase (ALP) and gamma-glutamyl transferase (GGT) may also be mildly elevated, reflecting liver inflammation, while bilirubinemia often exhibits a disproportionate rise in conjugated or unconjugated bilirubin depending on the underlying cause. Distinguishing these markers aids in differentiating hepatocellular damage from disorders affecting bilirubin clearance such as hemolysis or cholestasis.
Treatment Strategies: Distinct Approaches
Hepatitis treatment strategies primarily focus on antiviral medications, immunosuppressants, and lifestyle changes to reduce liver inflammation and prevent disease progression. Bilirubinemia management targets the underlying causes, such as hemolysis or bile duct obstruction, often involving phototherapy, exchange transfusions, or surgical interventions. Distinct therapeutic approaches reflect the different pathophysiologies of hepatitis's viral or autoimmune etiology versus bilirubinemia's metabolic or obstructive origins.
Potential Complications and Prognosis Comparison
Hepatitis can lead to severe liver complications such as cirrhosis, liver failure, and hepatocellular carcinoma, often requiring long-term management and potentially liver transplantation for prognosis improvement. Bilirubinemia, characterized by elevated bilirubin levels, primarily indicates underlying liver dysfunction or hemolysis and may result in kernicterus in neonates or chronic jaundice if untreated, with prognosis heavily dependent on the cause and timely intervention. Comparing both conditions, hepatitis poses a higher risk of progressive liver damage and systemic complications, while bilirubinemia's impact varies widely, ranging from benign transient states to critical neurological damage.
Prevention and Long-Term Management Tips
Preventing hepatitis involves vaccination, practicing safe needle use, avoiding contaminated food and water, and maintaining proper hygiene to reduce viral transmission. Long-term management of hepatitis includes regular liver function monitoring, adherence to antiviral treatments, and lifestyle modifications such as a balanced diet and abstaining from alcohol to prevent liver damage. In contrast, managing bilirubinemia centers on identifying and treating underlying causes, ensuring adequate hydration, and monitoring bilirubin levels to prevent complications like kernicterus in severe cases.
Hepatitis Infographic
 libterm.com
libterm.com