Concurrent processes enable multiple tasks to run simultaneously, improving system efficiency and performance. This approach is essential in modern computing, where multitasking and responsiveness are crucial. Explore the rest of the article to understand how concurrent execution can enhance your applications.
Table of Comparison
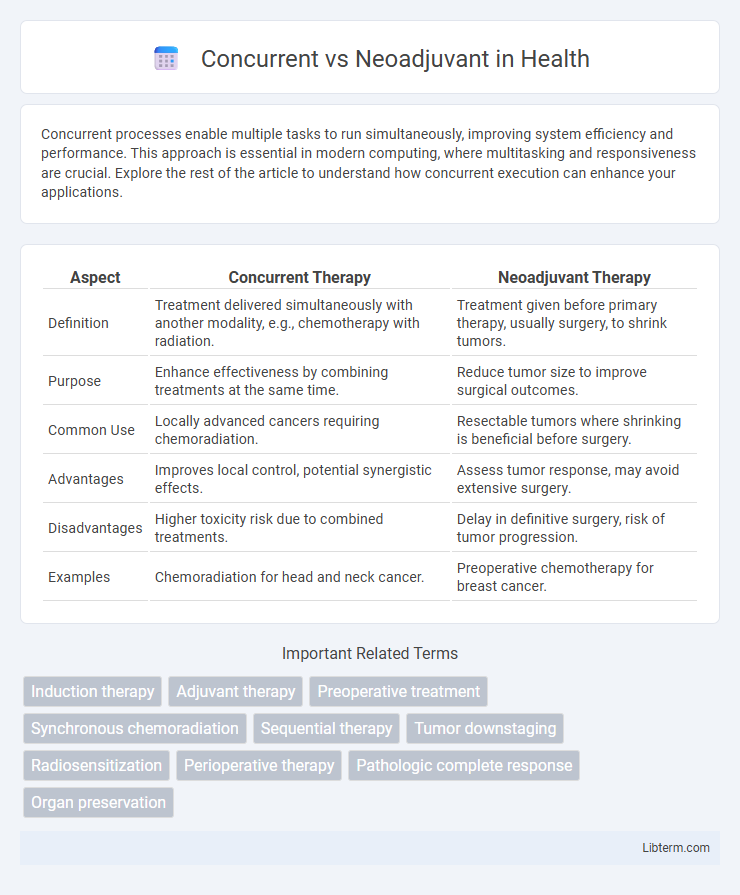
| Aspect | Concurrent Therapy | Neoadjuvant Therapy |
|---|---|---|
| Definition | Treatment delivered simultaneously with another modality, e.g., chemotherapy with radiation. | Treatment given before primary therapy, usually surgery, to shrink tumors. |
| Purpose | Enhance effectiveness by combining treatments at the same time. | Reduce tumor size to improve surgical outcomes. |
| Common Use | Locally advanced cancers requiring chemoradiation. | Resectable tumors where shrinking is beneficial before surgery. |
| Advantages | Improves local control, potential synergistic effects. | Assess tumor response, may avoid extensive surgery. |
| Disadvantages | Higher toxicity risk due to combined treatments. | Delay in definitive surgery, risk of tumor progression. |
| Examples | Chemoradiation for head and neck cancer. | Preoperative chemotherapy for breast cancer. |
Introduction to Concurrent and Neoadjuvant Therapies
Concurrent therapy involves administering treatments such as chemotherapy and radiation simultaneously to enhance the therapeutic effect on cancer cells, optimizing tumor control and survival rates. Neoadjuvant therapy refers to treatments given before the primary intervention, typically surgery, to reduce tumor size and improve operability while assessing tumor responsiveness. Both approaches are critical in multidisciplinary cancer management, contributing distinct advantages depending on tumor type, stage, and patient condition.
Definitions: What Is Concurrent Therapy?
Concurrent therapy refers to the simultaneous administration of chemotherapy and radiation treatment to enhance the effectiveness against cancer cells by exploiting their combined cytotoxic effects. This approach aims to maximize tumor control by targeting cancer through two modalities at the same time, often improving local control and survival rates in cancers such as head and neck, cervical, and lung cancers. In contrast, neoadjuvant therapy is given before the primary treatment, typically surgery, to shrink tumors and improve surgical outcomes.
Understanding Neoadjuvant Therapy
Neoadjuvant therapy involves administering treatments such as chemotherapy, radiation, or hormonal therapy before the primary intervention, typically surgery, to shrink tumors and improve surgical outcomes. This approach enhances the likelihood of complete tumor removal, reduces tumor size, and may address micrometastatic disease early in the treatment course. Understanding the timing and purpose of neoadjuvant therapy is crucial for optimizing cancer management and improving patient prognosis compared to concurrent treatments given simultaneously with other therapies.
Key Differences Between Concurrent and Neoadjuvant Approaches
Concurrent therapy involves administering chemotherapy simultaneously with radiation to enhance treatment efficacy against tumors, while neoadjuvant therapy provides chemotherapy or radiation before the main treatment, typically surgery, to shrink tumors and improve surgical outcomes. Key differences include timing, with concurrent therapy being simultaneous, and neoadjuvant being sequential, and their primary goals, where concurrent aims to boost the immediate effect of radiation, and neoadjuvant focuses on tumor reduction before surgery. Both approaches are selected based on cancer type, stage, and patient response, impacting overall treatment strategy and prognosis.
Indications for Concurrent Therapy
Concurrent therapy is primarily indicated for locally advanced cancers where simultaneous administration of chemotherapy and radiation enhances tumor control by sensitizing cancer cells to radiation. This approach is commonly used in head and neck squamous cell carcinoma, cervical cancer, and non-small cell lung cancer to improve overall survival and preserve organ function. The indication for concurrent therapy is often based on tumor stage, patient performance status, and evidence of potential radiosensitization benefit.
Indications for Neoadjuvant Therapy
Neoadjuvant therapy is primarily indicated for patients with locally advanced cancers, aiming to reduce tumor size before surgical intervention to improve operability and increase the likelihood of complete resection. It is often recommended in breast cancer, esophageal cancer, and rectal cancer cases where tumor downstaging can enhance surgical outcomes and facilitate organ preservation. This approach is beneficial in tumors with high risk of micrometastatic disease to improve long-term survival by addressing systemic disease early in the treatment course.
Efficacy: Comparing Treatment Outcomes
Concurrent chemoradiotherapy demonstrates higher efficacy by delivering chemotherapy simultaneously with radiation, enhancing tumor radiosensitivity and improving local control rates. Neoadjuvant therapy, administered prior to surgery, effectively reduces tumor size and addresses micrometastatic disease, potentially increasing resectability and long-term survival. Clinical studies indicate concurrent therapy yields better overall survival in locally advanced cancers, while neoadjuvant approaches benefit specific tumor types with extensive regional involvement.
Side Effects and Toxicity Profiles
Concurrent chemoradiation typically results in higher acute toxicity, including severe mucositis, hematologic suppression, and gastrointestinal effects, due to simultaneous administration of chemotherapy and radiation. Neoadjuvant therapy, given before radiation or surgery, often shows a more manageable side effect profile with fewer overlapping toxicities but can delay definitive treatment and occasionally lead to cumulative toxicity. Understanding these differences is crucial for tailoring treatment plans to minimize adverse effects while maximizing therapeutic efficacy in cancer management.
Patient Selection Criteria
Patient selection criteria for concurrent chemoradiotherapy emphasize tumor stage, performance status, and organ function to ensure tolerance to simultaneous treatment toxicity. Neoadjuvant therapy candidates are typically chosen based on tumor resectability, potential for downstaging, and absence of distant metastases to improve surgical outcomes. Biomarkers, patient comorbidities, and tumor genetic profiles also play an increasing role in optimizing personalized treatment strategies in both approaches.
Future Trends and Emerging Research
Future trends in cancer treatment are increasingly focused on optimizing the timing and combination of therapies, with emerging research exploring the efficacy of concurrent chemoradiotherapy versus neoadjuvant approaches. Advances in molecular profiling and precision medicine are driving personalized treatment plans that integrate immunotherapy and targeted agents alongside traditional modalities. Ongoing clinical trials aim to identify biomarkers that predict response to concurrent or neoadjuvant regimens, potentially improving survival outcomes and minimizing toxicity in cancers such as non-small cell lung cancer and locally advanced rectal cancer.
Concurrent Infographic
 libterm.com
libterm.com