Hemorrhage refers to the excessive or uncontrolled bleeding that can occur internally or externally, often resulting from injury, surgery, or medical conditions affecting blood vessels. Prompt recognition and treatment are crucial to prevent complications such as hypovolemic shock or organ damage. Explore the rest of this article to understand the causes, symptoms, and effective management strategies for hemorrhage.
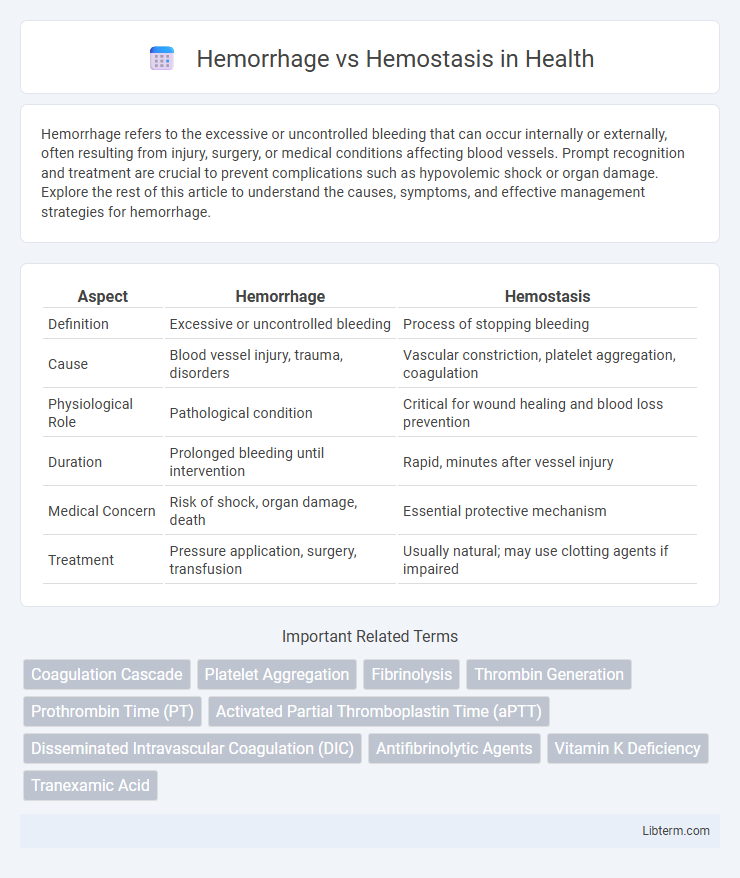
Table of Comparison
| Aspect | Hemorrhage | Hemostasis |
|---|---|---|
| Definition | Excessive or uncontrolled bleeding | Process of stopping bleeding |
| Cause | Blood vessel injury, trauma, disorders | Vascular constriction, platelet aggregation, coagulation |
| Physiological Role | Pathological condition | Critical for wound healing and blood loss prevention |
| Duration | Prolonged bleeding until intervention | Rapid, minutes after vessel injury |
| Medical Concern | Risk of shock, organ damage, death | Essential protective mechanism |
| Treatment | Pressure application, surgery, transfusion | Usually natural; may use clotting agents if impaired |
Introduction to Hemorrhage and Hemostasis
Hemorrhage refers to the excessive or uncontrolled bleeding resulting from damaged blood vessels, posing significant risks such as hypovolemic shock and organ failure. Hemostasis is the physiological process that prevents and stops bleeding by forming clots through vascular constriction, platelet aggregation, and coagulation cascades. Effective hemostasis is critical in maintaining vascular integrity and preventing hemorrhagic complications during injury or surgery.
Definition of Hemorrhage
Hemorrhage is the medical condition characterized by excessive or uncontrolled bleeding due to the rupture of blood vessels, which can result in significant blood loss and potentially lead to hypovolemic shock or death. This condition can be classified into external or internal hemorrhage based on the bleeding location. Understanding hemorrhage is critical for timely intervention and management to prevent severe complications and support hemostasis, the physiological process that stops bleeding and maintains vascular integrity.
Definition of Hemostasis
Hemostasis is the physiological process that stops bleeding at the site of an injured blood vessel through vascular constriction, platelet plug formation, and blood coagulation. It involves a complex interaction between blood vessels, platelets, and coagulation factors to maintain blood fluidity and prevent excessive blood loss. Hemorrhage, in contrast, is the excessive or uncontrolled bleeding resulting from the failure or disruption of normal hemostatic mechanisms.
Types and Causes of Hemorrhage
Hemorrhage is the escape of blood from ruptured blood vessels, classified into external, internal, and internal bleeding into body cavities. Common causes include trauma, vascular diseases like aneurysms, coagulation disorders, and hypertension, leading to vessel rupture or impaired clot formation. In contrast, hemostasis is the physiological process that stops bleeding through vascular spasm, platelet plug formation, and coagulation, maintaining blood vessel integrity.
Mechanisms of Hemostasis
Hemostasis involves a complex series of mechanisms including vascular spasm, platelet aggregation, and coagulation cascade activation to prevent hemorrhage. Platelets adhere to the damaged endothelium, releasing granules that promote further platelet activation and fibrin mesh formation, stabilizing the clot. Coagulation factors are sequentially activated through intrinsic and extrinsic pathways, culminating in the conversion of fibrinogen to fibrin, which reinforces the platelet plug and achieves vessel repair.
Clinical Significance: Hemorrhage vs Hemostasis
Hemorrhage involves uncontrolled bleeding that can lead to hypovolemic shock, organ failure, or death if not promptly managed, making rapid identification and intervention critical in clinical settings. Hemostasis is the physiological process that stops bleeding through vasoconstriction, platelet aggregation, and coagulation cascades, essential for wound healing and preventing excessive blood loss during surgery or trauma. Proper balance between hemorrhage and hemostasis is vital for patient outcomes, with clinical protocols often targeting enhanced hemostatic mechanisms to control hemorrhage and improve recovery.
Diagnostic Approaches for Hemorrhagic Disorders
Diagnostic approaches for hemorrhagic disorders emphasize differentiating between hemorrhage and effective hemostasis by evaluating coagulation parameters, platelet function, and vessel integrity. Laboratory tests such as prothrombin time (PT), activated partial thromboplastin time (aPTT), bleeding time, and platelet count help identify abnormalities in clotting factors and platelet activity. Advanced diagnostic tools including thromboelastography (TEG) and genetic testing provide detailed insights into coagulation pathways and inherited bleeding conditions.
Management and Treatment Strategies
Management of hemorrhage prioritizes rapid identification and control of bleeding through techniques such as direct pressure, tourniquets, and surgical intervention including vessel ligation or embolization. Hemostasis involves the use of pharmacological agents like antifibrinolytics (e.g., tranexamic acid), topical hemostatic agents, and coagulation factor replacement to stabilize clot formation and prevent further blood loss. Advanced treatment strategies integrate blood transfusions, hemodynamic support, and monitoring of coagulation parameters to balance bleeding control and prevent thrombosis.
Complications Associated with Impaired Hemostasis
Impaired hemostasis can lead to severe complications such as uncontrolled hemorrhage, which increases the risk of hypovolemic shock and organ failure due to excessive blood loss. Patients with clotting factor deficiencies or platelet dysfunction are particularly susceptible to persistent bleeding and delayed wound healing. These complications necessitate prompt medical intervention to restore hemostatic balance and prevent life-threatening outcomes.
Prevention and Future Directions
Effective prevention of hemorrhage involves strategies such as early detection of bleeding risks, use of anticoagulant reversal agents, and implementation of minimally invasive surgical techniques. Hemostasis advancements focus on developing targeted hemostatic agents, such as recombinant clotting factors and novel platelet substitutes, to enhance blood clot formation and stability. Future directions emphasize personalized medicine approaches, integrating genetic and biomarker profiling to optimize hemorrhage management and improve patient outcomes.
Hemorrhage Infographic
 libterm.com
libterm.com