Anorexia is a serious eating disorder characterized by an intense fear of gaining weight and a distorted body image, leading to extreme food restriction and significant weight loss. It affects both physical health and mental well-being, causing complications such as malnutrition, heart issues, and anxiety. Discover essential information on recognizing symptoms, causes, and effective treatments to support your recovery journey in the full article.
Table of Comparison
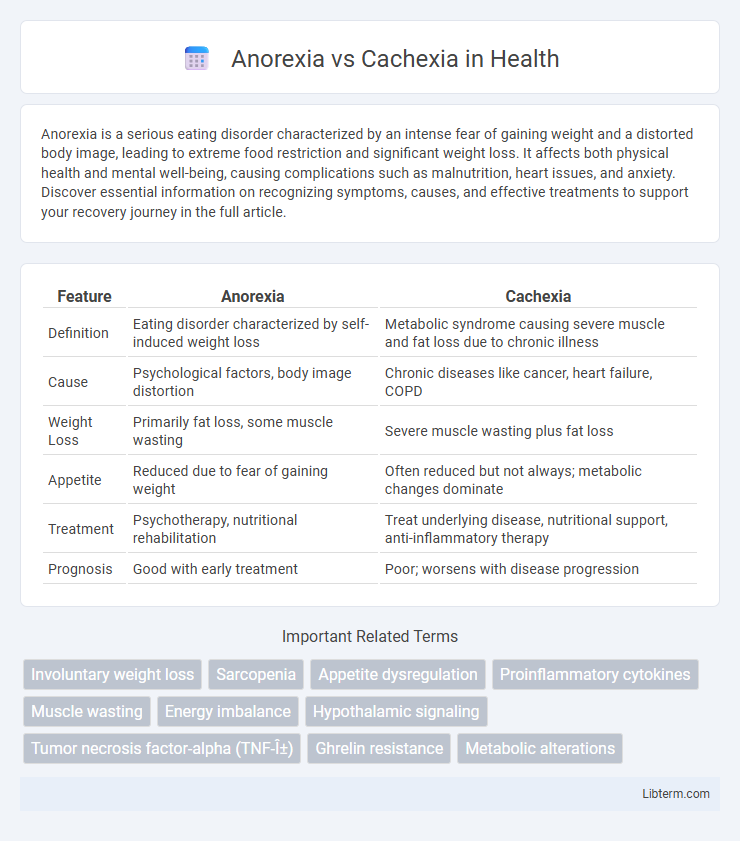
| Feature | Anorexia | Cachexia |
|---|---|---|
| Definition | Eating disorder characterized by self-induced weight loss | Metabolic syndrome causing severe muscle and fat loss due to chronic illness |
| Cause | Psychological factors, body image distortion | Chronic diseases like cancer, heart failure, COPD |
| Weight Loss | Primarily fat loss, some muscle wasting | Severe muscle wasting plus fat loss |
| Appetite | Reduced due to fear of gaining weight | Often reduced but not always; metabolic changes dominate |
| Treatment | Psychotherapy, nutritional rehabilitation | Treat underlying disease, nutritional support, anti-inflammatory therapy |
| Prognosis | Good with early treatment | Poor; worsens with disease progression |
Definition of Anorexia
Anorexia is a medical condition characterized by a significant loss of appetite or inability to eat, often leading to severe weight loss and malnutrition. It differs from cachexia, which is a complex metabolic syndrome associated with chronic illness, marked by muscle wasting and systemic inflammation. Understanding anorexia as a primary appetite disorder helps distinguish it from cachexia, which involves multifactorial metabolic disruptions beyond reduced food intake.
Definition of Cachexia
Cachexia is a complex metabolic syndrome characterized by severe muscle wasting, weight loss, and systemic inflammation, often associated with chronic illnesses such as cancer, heart failure, or chronic kidney disease. Unlike anorexia, which primarily involves reduced appetite and food intake, cachexia involves a multifactorial imbalance of anabolic and catabolic processes leading to significant muscle degradation despite adequate nutrition. This syndrome significantly impacts patient morbidity and mortality by impairing physical function and response to treatment.
Key Differences Between Anorexia and Cachexia
Anorexia primarily involves a loss of appetite leading to reduced food intake, while cachexia is characterized by a complex metabolic syndrome causing severe muscle wasting and weight loss despite normal or increased food consumption. Anorexia often results from psychological factors or illness-induced appetite changes, whereas cachexia is associated with chronic diseases like cancer, heart failure, or chronic kidney disease, involving systemic inflammation and catabolic processes. Unlike anorexia, cachexia cannot be fully reversed by nutritional support due to its underlying pathophysiology targeting muscle and fat tissue degradation.
Causes and Risk Factors
Anorexia primarily arises from psychological factors such as depression, anxiety, or eating disorders, while cachexia is caused by underlying chronic illnesses like cancer, heart failure, or chronic kidney disease. Risk factors for anorexia include body image disturbances, low self-esteem, and exposure to societal pressures, whereas cachexia risk factors emphasize systemic inflammation, metabolic derangements, and advanced stage disease. Both conditions result in significant weight loss, but their distinct etiologies necessitate different approaches to diagnosis and treatment.
Clinical Signs and Symptoms
Anorexia presents primarily with reduced appetite, significant weight loss, and fatigue, often accompanied by gastrointestinal disturbances like nausea and early satiety. Cachexia involves severe muscle wasting, systemic inflammation, and metabolic imbalances, characterized by unintentional weight loss despite adequate nutritional intake. Both conditions exhibit weakness and reduced functional status, but cachexia is marked by elevated pro-inflammatory cytokines and altered energy metabolism.
Pathophysiology Overview
Anorexia involves a decrease in appetite due to dysfunction in the hypothalamic regulation of hunger signals, often linked to psychological factors or systemic illnesses, resulting in reduced food intake and energy imbalance. Cachexia is characterized by complex metabolic alterations including increased inflammatory cytokines such as TNF-a, IL-6, and interferon-gamma, leading to muscle protein catabolism, fat loss, and impaired anabolism despite adequate nutrition. Unlike anorexia, cachexia involves a hypercatabolic state driven by chronic diseases like cancer or chronic heart failure, causing progressive weight loss and muscle wasting independent of nutritional intake.
Diagnostic Criteria and Assessment
Anorexia is primarily diagnosed using clinical evaluation based on reduced appetite and food intake, often linked to psychiatric conditions such as anorexia nervosa, with assessment tools including the Eating Disorder Examination and DSM-5 criteria. Cachexia is identified by unintentional weight loss greater than 5% over 12 months or less, with criteria emphasizing muscle wasting and systemic inflammation, assessed using parameters like weight history, muscle mass measurement (e.g., bioelectrical impedance analysis), and biomarkers such as C-reactive protein. Differentiating anorexia from cachexia involves analyzing appetite status, inflammatory markers, and muscle mass depletion alongside comprehensive nutritional and metabolic assessments.
Treatment Approaches and Management
Treatment approaches for anorexia primarily involve nutritional rehabilitation, psychological therapy such as cognitive-behavioral therapy, and sometimes pharmacological interventions to address underlying psychiatric conditions. Cachexia management focuses on treating the underlying chronic illness, employing nutritional support combined with anti-inflammatory and anabolic agents like corticosteroids or selective androgen receptor modulators to counteract muscle wasting. Both conditions require multidisciplinary care to optimize patient outcomes and improve quality of life.
Prognosis and Complications
Anorexia typically has a variable prognosis depending on early diagnosis and treatment compliance, but complications such as severe malnutrition, cardiac arrhythmias, and osteoporosis significantly impact long-term outcomes. Cachexia, often associated with chronic illnesses like cancer or heart failure, presents a poorer prognosis due to progressive muscle wasting, systemic inflammation, and multi-organ dysfunction. Both conditions increase morbidity and mortality, but cachexia's irreversible metabolic alterations generally lead to a more fatal clinical course.
Prevention and Patient Support
Effective prevention of anorexia and cachexia involves early nutritional assessment and intervention tailored to individual patient needs, emphasizing calorie-dense and nutrient-rich diets. Patient support includes multidisciplinary approaches combining psychological counseling, symptom management, and physical therapy to maintain muscle mass and improve quality of life. Continuous monitoring and personalized care plans are essential to address underlying causes and prevent progression of both conditions.
Anorexia Infographic
 libterm.com
libterm.com